Welcome to the brief update of my hospital carers discharge toolkit meeting. I chair this meeting every two months with support of the carer centres and some hospitals.
The London Hospital discharge toolkit aims to provide a collaborative platform where unpaid carers, hospital carer leads and carer centres can work together to:
- Enhance support for unpaid carers of patients using hospital services.
- Improve communication and engagement between hospital staff and unpaid carers especially during patient discharge.
- Identify and address the needs and concerns of carers within the hospital setting.
- Share ways to implement London Hospital discharge toolkit to ensure carers are recognized, supported, and actively involved in the care journey of their loved ones while in hospital.
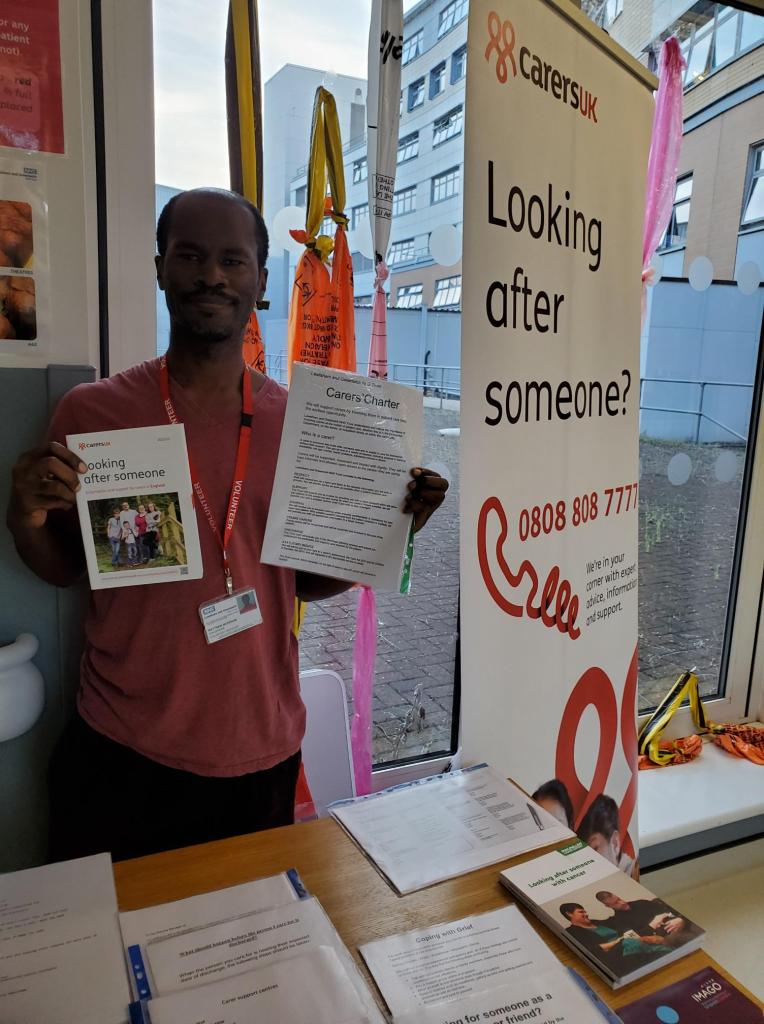
For January 2025 meeting, we focused on the engagement of unpaid carers with hospital services, particularly in the context of the London Hospital Discharge Toolkit. The group discussed challenges such as the lack of hospital staff awareness about carers, the need for a more proactive approach to identifying carers, and the importance of securing leadership buy-in and higher-level meetings with hospital directors. The meeting also covered the progress of various initiatives, including carer awareness training, the introduction of carer awareness badges, and the potential for a carers stall every month to promote services and increase referrals, which is something I usually try and do as a volunteer every now and then while promoting Carers UK, Macmillan Cancer Support and Parkinsons UK.
The January meeting saw a good turnout from representatives of carers centers across London, although not many carer hospital reps. I encouraged participants to introduce themselves and share their experiences including Sutton Carers Center, NHS England, unpaid carers, representatives from Queen Elizabeth Hospital over in Greenwich, Camden Carers Center, Lewisham University Hospital, Barnett Carers, Harrow Carers, and Carers Hub Lambeth. The conversation from Nhs England, was on expected updates on the work happening nationally regarding unpaid carers.
NHS 10-Year Plan and Unpaid Carers
There were discussions on the ongoing 10-year plan for the NHS, led by the national team, which includes engagement with carers. NHS England mentioned that the plan is expected to be released in the spring and will likely include policy directions for unpaid carers. Also NHS England highlighted the importance of unpaid carers being represented in the strategy groups. However unpaid carers expressed concern about how to influence the local level. There was a suggestion of using the ‘Workshop in a Box’ initiative, which is open until February 14th. Another suggestion was for carers to engage with the local ICB and place boards, but this is proving difficult.
Hospital Engagement and Carer Support
I expressed a desire for more engagement with local hospitals, particularly in the southwest and north regions. I also suggested that introducing the heads of ICBS could help facilitate this. NHS England felt this important to continue sending links to the heads of ICBs. Some hospital NHS trusts, admitted that they haven’t been able to progress the issue of carer engagement due to team changes and a lack of resources. It was mentioned that they are trying to get carers flagged on the electronic patient record system. Unpaid carers at the group offered support, however I emphasized the importance of hearing the honest challenges and successes, and suggested that getting engagement from ICBS could be beneficial.
Hospital Discharge Referral Challenges

In the meeting, a carer centre discussed their challenges in receiving hospital discharge referrals from their local hospital, despite their efforts to engage with the hospital staff. They suggested that the issue might be due to a lack of training for hospital staff to recognize and support carers. Another Carer centre shared their experience of using carer awareness badges to prompt staff to recognize carers, but acknowledged that this might not be feasible for all teams due to funding constraints. The group agreed that securing leadership buy-in and higher-level meetings with hospital directors could be a potential solution to some of the problems.
Improving Carer Identification in Hospitals
Our group also discussed the challenges of identifying carers in hospitals and the need for a more proactive approach. Carer centres highlighted that the identification of carers should ideally come from the hospital, but currently, all referrals seem to be identified internally.

Carer centre reps added that while GP referrals have improved, they are not coming directly from the hospital. Unpaid carers also emphasized the need for a soft sell approach by hospital staff to encourage carers to identify themselves. A carer centre representative suggested that carers might be self-referring after receiving information from the hospital. Another carer centre representative shared her experience working with a charity, where she encountered resistance and confusion among hospital staff and carers about the concept of unpaid carers. This is because even carers themselves do not recognise themeselves as unpaid carers which might seem fine until they need resources or do not know about their rights.
The group agreed on the need for a more effective and consistent approach to identifying unpaid carers.
Care Awareness Training Progress Update
Carer centre reported on the progress of the carer awareness training, which has been well-received by nearly 80 attendees over 10 sessions. They also mentioned the introduction of carer awareness badges to increase visibility and conversation about the program. The carer centre highlighted the importance of individual conversations with key contacts, such as an unpaid carer who supports the project.
The carer centre also discussed ongoing collaborations with other carer centers and the redesign of communications to simplify the referral process. I expressed interest in Camden carer centre’s experience on the update on Camden Carers’ activities, including successful engagement with GPs and some hospital teams, but they also noted challenges in engaging with hospitals.
Carers Engagement and Support Strategies
In the meeting, I discussed the challenges of engaging with carers and the potential for a carers stall every month to promote services and increase referrals. I also mentioned the need for increased referrals from the hospital and shared contact details for further engagement. A carer centre shared their experiences with a carers stall and the challenges of reaching out to many wards. They also mentioned their plans to meet ward managers and potentially recruit volunteers to help. Another representative discussed the carers passports and the support network for carers, and suggested revisiting the system every year or six months. The group agreeded to keep each other updated on carers-related matters.
This is the brief update for January’s meeting until the next one in March
