By Matthew McKenzie Cygnet Carer Ambassador
Thursday 8th May 2025 | 10:00 – 16:30
National Conference Centre and Motorcycle Museum, Birmingham

Yes, as you can tell by the date of the conference, this blog took ages to write, it was not helped that my computer decided to die on me and I had to re-write certain sections again.
Anyway, attending the Cygnet Annual Nursing Conference and Awards 2025 as a Carer Ambassador wasn’t just informative it was empowering. As someone whose life has been shaped by navigating the health system with a loved one, this event felt like a shared space where lived experience wasn’t just welcomed it was valued, where we at least attended and networked
Learning about nursing and nurse wellbeing.
This conference didn’t just give space for clinical frameworks and policy updates, it gave space for people. And for me, that’s what made the eveent truly powerful. Many presenters talked about their journeys, from early support roles to leadership. I found myself nodding along the main speaker David Wilmot recalled standing awkwardly in a ward, unsure of what to say to someone in distress. That honesty resonated with my own journey supporting loved ones through their darkest days, I was unsure about my own role.
What I witnessed at this conference was systems that are learning to listen better to staff, service users, and crucially, carers. The word “co-production” wasn’t just jargon. It was active, present, and visible in every story shared and every framework described.
What the Day Looked Like – Agenda Highlights
Here’s how the day unfolded, each session echoing the deep need for care, compassion, and co-production:
🕙 10:00 – Registration
🕥 10:15 – Welcome & Introductions



David Wilmot, Director of Nursing, Cygnet Group
David Wilmot was more than just a speaker at this year’s conference—he was the anchoring voice and spirit of the day. As Director of Nursing, he carried both authority and approachability, creating a space where nurses, carers, students, and leaders felt equally welcome.

Throughout the event, David returned to the microphone to introduce sessions, celebrate achievements, and frame the evolving narrative of nursing within Cygnet. His tone was often one of pride but not the self-congratulatory kind. Instead, it was a deep appreciation for the workforce, and a humility that recognized how much there still is to do to support and uplift nurses at every level.
As someone who has supported a loved one through complex care, I was especially moved when David spoke about the human side of practice how safety, compassion, and professional integrity must walk hand in hand. He didn’t shy away from the reality of burnout, staffing pressures, or the emotional toll of nursing. But he countered that with a call to action: to lead with purpose, to connect with others, and to always remember why we do this work.
David’s presence also gave shape to Cygnet’s Nursing Strategy 2025–2027. He described the new direction not just in policy terms but in values. What stood out was his emphasis on co-production, inclusion, and professional development, reinforcing the belief that every nurse and carer has a voice worth hearing.

In short, David Wilmot embodied visionary leadership with a personal touch and his words resonated with everyone in the room, including those of us who’ve seen nursing from the other side of the care relationship.
10:30 – Keynote: Future of Nursing in the UK
Patricia Marquis, Executive Director, Royal College of Nursing
Patricia Marquis opened her address by reflecting on her journey in nursing since the 1980s and her long-standing commitment to improving the profession through the RCN. She emphasized the deep value and unique impact of nurses in society, stressing that if nurses led the world, it would be a better place. Patricia highlighted the challenges facing the profession, such as the high dropout rates among nursing students, a 43% attrition rate within the first 10 years of practice, and declining applications to nursing programs. She advocated for structured support for newly qualified nurses, mental health investment, compassionate leadership, and the recognition of emotional intelligence as central to effective care. Patricia also discussed policy engagement, the importance of workforce planning, and the RCN’s efforts to influence national reforms.
10:40 – Keynote: Leadership and Nursing
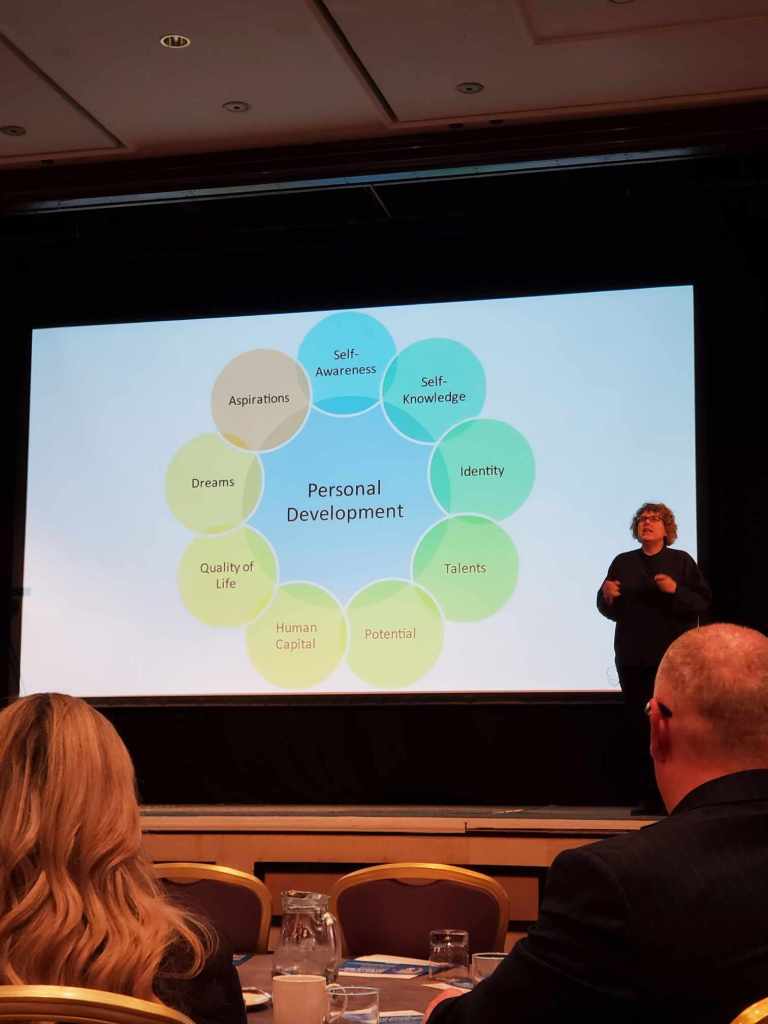
Professor Irene Gray, Independent Coach, former Chief Nurse
Professor Irene Gray delivered a deeply personal and reflective address that centered on the theme of authenticity and courage in leadership. Drawing on her own journey from a nurse and Chief Nurse to becoming a coach, she spoke candidly about the challenges of staying true to one’s values in a system that can sometimes feel unforgiving. Irene underscored the emotional weight nurses carry and the personal cost of silence, especially in situations where speaking up feels risky.
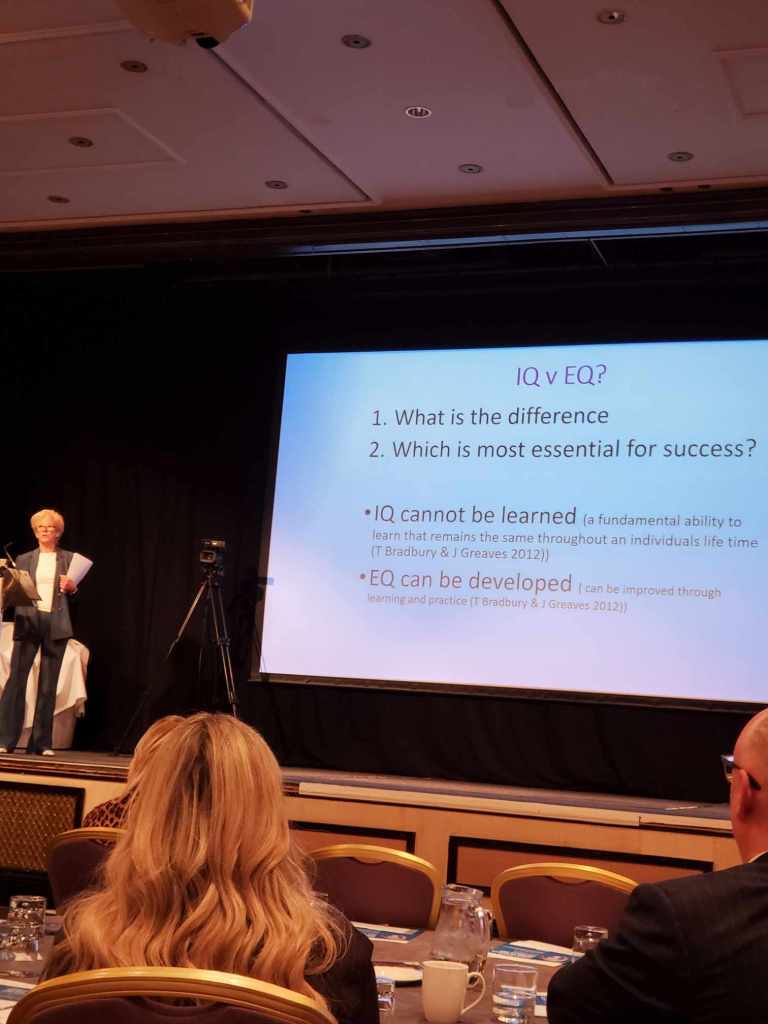

She encouraged attendees to remain anchored in their integrity and to understand that leadership isn’t about perfection but about connection, compassion, and accountability. Her reflections offered permission for vulnerability and reminded the audience that leadership and care are fundamentally human acts. Irene’s heartfelt delivery was both grounding and empowering, especially for those navigating the complexities of mental health and learning disability care.
11:00 – Keynote: Mental Health Nursing Overview
Rebecca Burgess-Dawson, National Clinical Lead (Mental Health), South West Yorkshire Partnership NHS FT
Rebecca Burgess-Dawson brought both clarity and urgency to her discussion on the evolving identity of mental health nursing. She spoke with conviction about the need to move away from outdated models of care that pathologise distress, instead advocating for a trauma-informed, socially aware approach that puts lived experience at the centre. Rebecca emphasised the value of relationships, humanity, and compassion in practice, challenging nurses to reflect on the real meaning of therapeutic work.
She explored how mental health nursing is uniquely positioned to lead system change calling for the profession to be bold, visible, and unafraid to challenge the status quo. There was a strong thread throughout her speech around restoring pride in the profession while also doing the necessary work of dismantling harmful or paternalistic legacies. Her powerful reflections inspired many, especially carers and lived experience representatives in the room, who saw in her vision a path toward more collaborative, healing-centred care.
11:40 – Quality Improvement: Diamond Framework
Joshua Tapp & Jacinta Fox, Cygnet Hospital Kewstoke

Joshua Tapp and Jacinta Fox offered a powerful example of authentic collaboration between staff and individuals with lived experience. Their joint presentation from Cygnet Hospital Kewstoke focused on building hope, connection, and recovery by challenging traditional hierarchies within mental health settings. Jacinta, speaking from lived experience, courageously shared her journey of mental health recovery, including the barriers she faced and what ultimately helped her begin to heal feeling listened to, being seen as a person, not a diagnosis.
Joshua, as a nurse and ally, highlighted how his practice has been transformed by listening to service users like Jacinta. Together, they illustrated what’s possible when staff work with rather than on people. Their dynamic reinforced the message that true recovery is relational, and that safety and progress are co-produced when trust and mutual respect are at the centre.
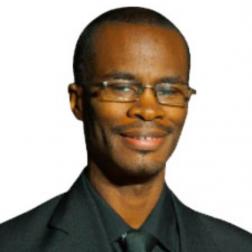
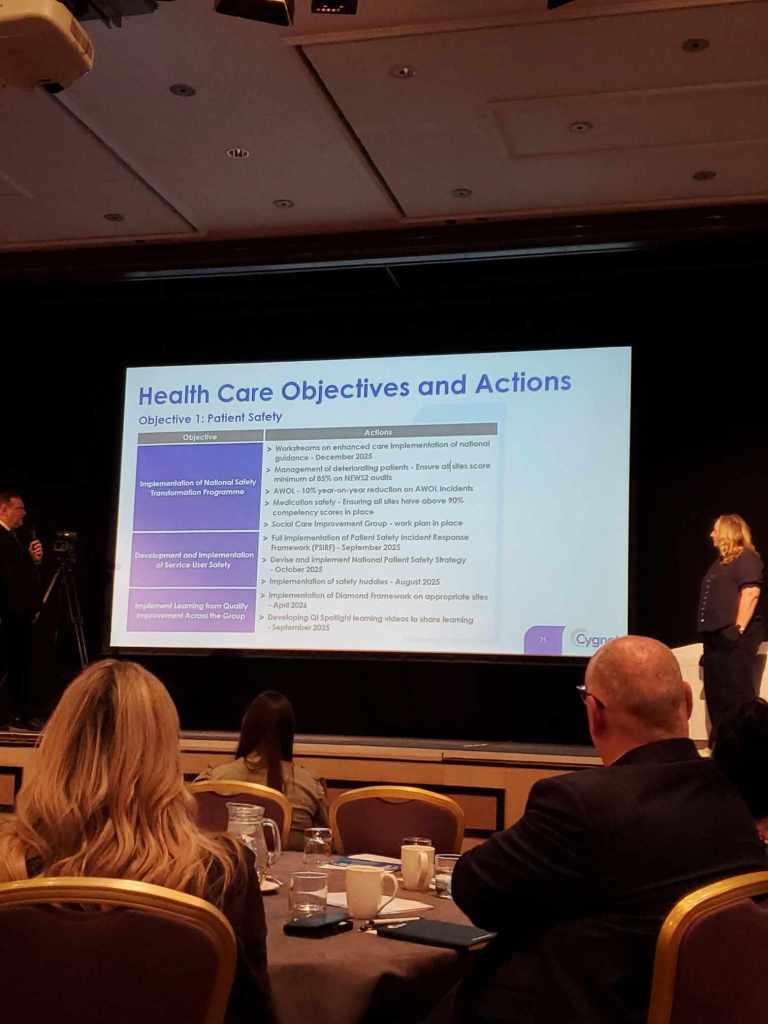
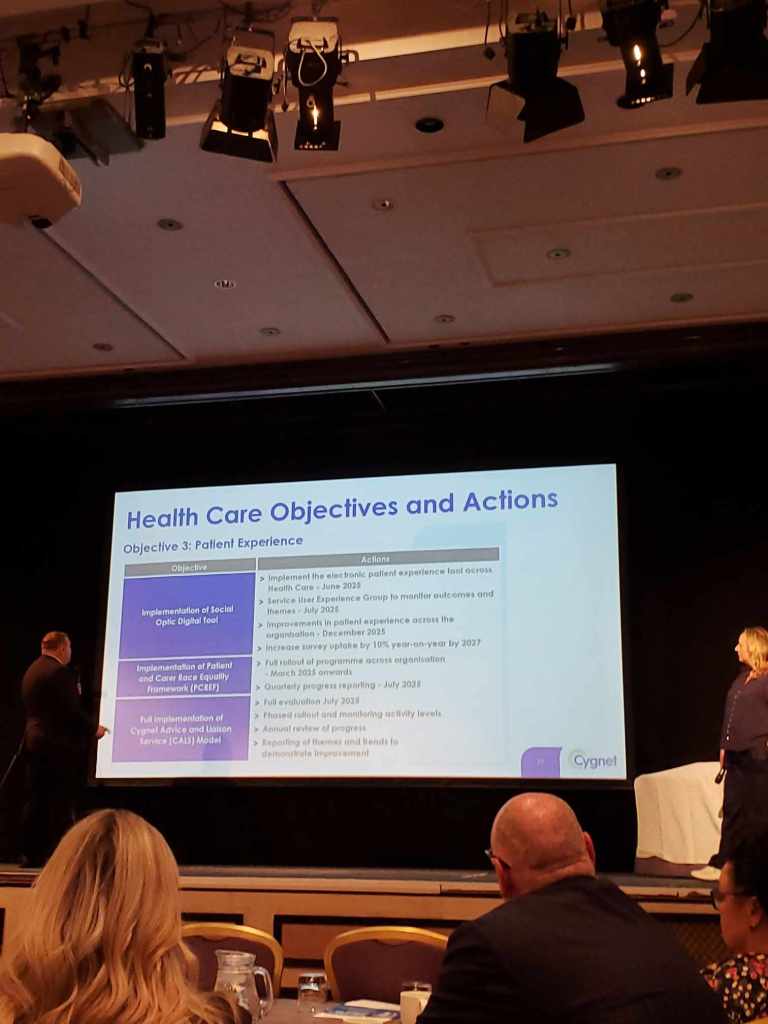
12:00 – Cygnet’s Nursing Strategy 2025–2027
Presented by Cygnet nursing leadership team
The Cygnet Nursing Leadership Team presented the new Nursing Strategy 2025–2027 with a clear, focused ambition: to move beyond the basics of clinical care and embed a culture of compassionate, evidence-informed, and recovery-oriented practice across every Cygnet service.
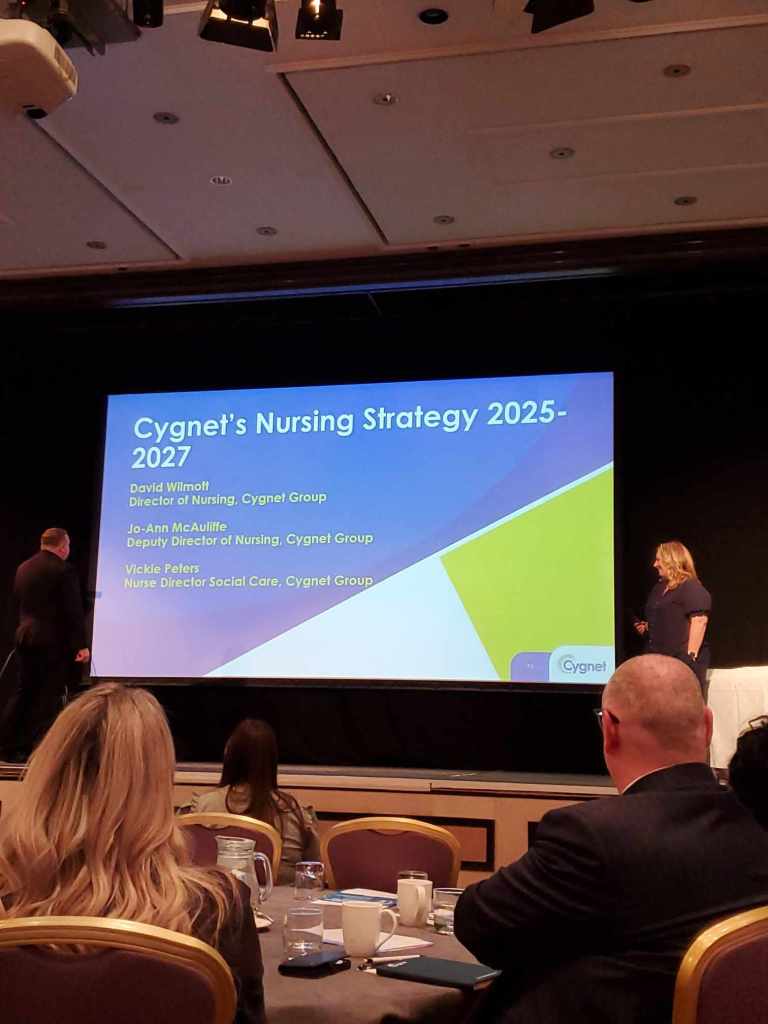
As someone with lived experience of caring, I found this session particularly affirming. It was clear that the leadership team had genuinely reflected on the voices of carers, patients, and front-line staff. They acknowledged that while clinical excellence remains essential, nursing is fundamentally about relationships being present, being human, and being consistent in care.
The strategy was built around core pillars, including:
Professional Development – investing in continuous learning and leadership for nurses at all levels.
Lived Experience and Co-production – recognising that those who use services, and those who care for them, have invaluable insights that must shape care.
13:00 – Lunch & Networking


13:00 – Keynote: Risk Planning & Safety Formulation
Natasha Bryant, Avon and Wiltshire Suicide Prevention Lead

Natasha Bryant’s session on Risk Planning and Safety Formulation was deeply impactful not just because of her expertise, but because of her humanity. As a carer, I’ve often seen risk management treated like a tick-box exercise. But Natasha reminded us that risk is not just clinical, it’s emotional, personal, and nuanced.
She emphasised “safety formulation” over “risk assessment.” This might sound like semantics, but it’s a fundamental shift. Instead of asking “How risky is this person?” we ask, “What do we know about this person that helps us understand their distress and how we can keep them safe?” It’s about collaborating, not policing. Listening, not labelling.
She introduced trauma-informed and compassion-focused approaches to suicide prevention, highlighting that many individuals who experience suicidal thoughts don’t necessarily want to die, they want to end pain. This understanding changes everything.
What I appreciated most was her validation that carers have crucial insights. She talked about relational safety how connections, routine, and being truly known by someone can offer more protection than any checklist. She also acknowledged the need to involve carers in safety planning, not sideline them.
This session made it clear that effective risk planning isn’t about control, it’s about partnership. It’s about knowing the person, understanding their story, and building plans together that feel supportive, not punitive.
13:20 – Keynote: Learning Disability Nursing – Has It Got a Future?
Caroline Harris-Birtles, Vickie Peters, Vicky Sandy-Davis
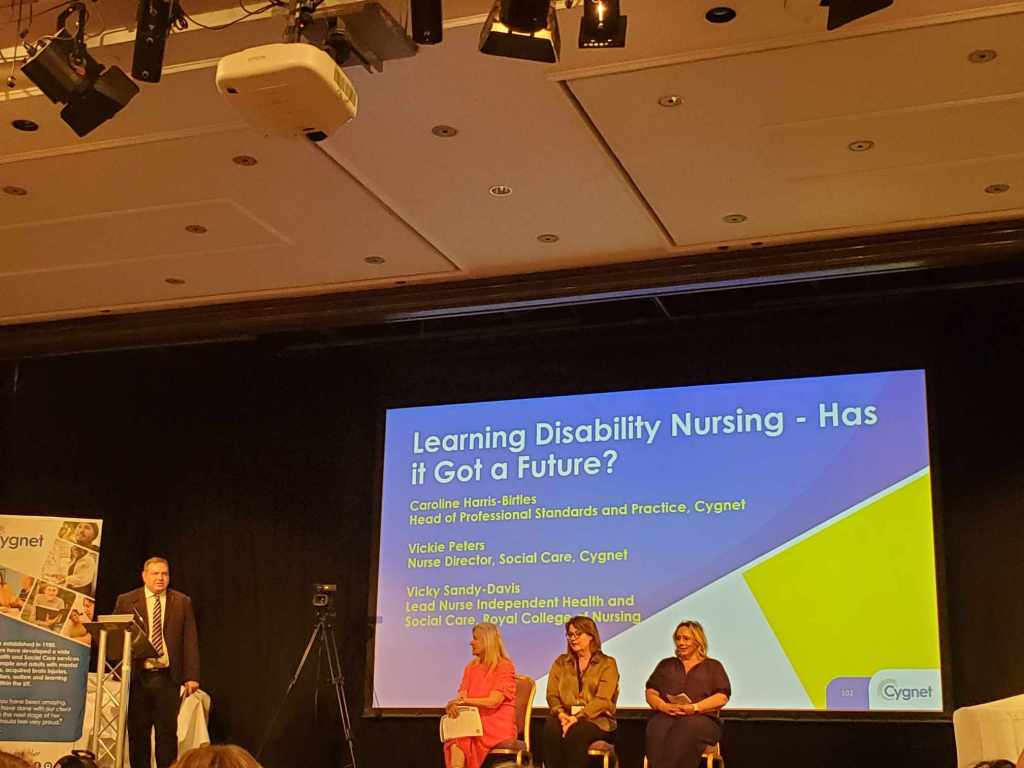
This session struck a powerful chord. Caroline Harris-Birtles, Vickie Peters, and Vicky Sandy-Davis didn’t just ask whether learning disability (LD) nursing has a future they made the case that it absolutely must. And as a carer, I couldn’t agree more.
They opened by highlighting the critical and often invisible role LD nurses play not just in care delivery but in advocacy, communication, and protecting human rights. I’ve witnessed firsthand how learning disability nurses act as translators between a world that moves too fast and people who need time, understanding, and dignity. Without them, people fall through the cracks.
The speakers reflected honestly on the challenges the profession faces: workforce shortages, under-recognition, and training pathways under threat. But instead of sounding defeated, they were energised. They championed the specialist skillset of LD nurses—relational, behavioural, sensory-aware, and trauma-informed and argued that these are not “soft skills” but lifesaving tools.
One point that stood out: the need for visibility. Many people don’t even realise LD nursing is a separate branch of the profession. This invisibility contributes to the very risk of extinction. The presenters called on all of us nurses, carers, services to advocate louder and educate better.
13:40 – Keynote: Advanced Nursing in the UK
Paula McLaren, Nursing and Midwifery Council

As a carer, I’ve often seen advanced nurses step into complex situations with clinical skill and human understanding that can make or break someone’s journey. That’s why Paula McLaren’s session on the evolution of advanced nursing in the UK felt not only timely but essential.
Paula spoke with clarity and conviction about the regulatory gaps that exist today. Unlike doctors, advanced nurses in the UK currently operate without formal NMC regulation tied to their advanced role. This lack of clarity, she explained, creates risks to public safety, inconsistent educational standards, and confusion for patients, carers, and professionals alike.
One of the most powerful takeaways was the data gap, we don’t even know how many advanced practitioners are working across the UK. As a carer, that’s frightening. These are professionals making life-altering decisions, often in community settings, and they deserve recognition, training, and standards to match the trust we place in them.
Paula walked us through the NMC’s staged work plan, starting with consultation and co-design of standards, with a long-term vision for clear routes into recognition and registration. She was honest: it won’t happen overnight. But it was heartening to hear that the NMC isn’t just aiming to catch up, it’s aiming to get this right for the future.
What resonated most was Paula’s insistence that advanced practice must be inclusive, recognising real-life experience, lived expertise, and those already working in advanced ways, even if they haven’t had the chance to do a Master’s degree. That means people like those supporting my family whose skills have been hard-earned in frontline care won’t be left behind.
14:00 – Keynote: Nurse Practitioner in the United States
Karen Johnson & Danielle Devereaux, Universal Health Services
As someone who’s spent years supporting a loved one through mental health and complex care systems here in the UK, hearing from Karen Johnson and Danielle Devereaux about the Nurse Practitioner (NP) model in the United States was like opening a window into another healthcare world one that feels both familiar and ambitiously evolved.
They painted a vivid picture of how NPs in the U.S. are not just clinicians, but leaders, educators, and innovators. These professionals are stepping into primary care roles, specialist practice, and even surgical and acute hospital teams, with prescribing rights, diagnostic authority, and autonomy that rivals that of physicians. It was both inspiring and a little sobering especially when reflecting on where the UK currently sits in comparison.
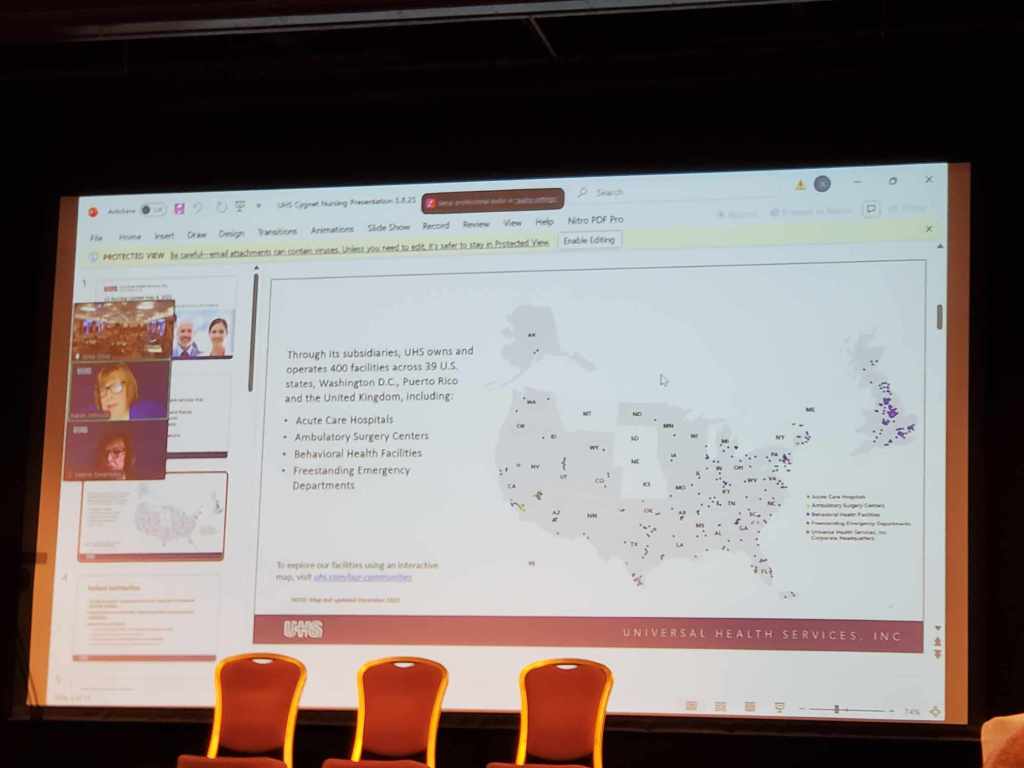
One point that struck me deeply was the structured educational pathway in the U.S.—Nurse Practitioners complete Master’s or Doctorate-level training, with standardised licensure that’s recognised across many states thanks to the Nursing Compact Agreement. For carers and service users, this means clarity: we know what an NP can do, and we know they’re accountable. That sense of security really matters.
Danielle spoke about the impact of NPs in mental health, particularly across underserved areas. As someone who’s seen care delayed because “the consultant’s not in until Thursday,” it was heartening to hear how NPs are filling critical gaps, especially in community and behavioural health services.
But this wasn’t just an American success story. Karen made it clear that their journey wasn’t without barriers, burnout, and political tension, particularly around scope of practice and recognition. That honesty made their accomplishments even more valuable.
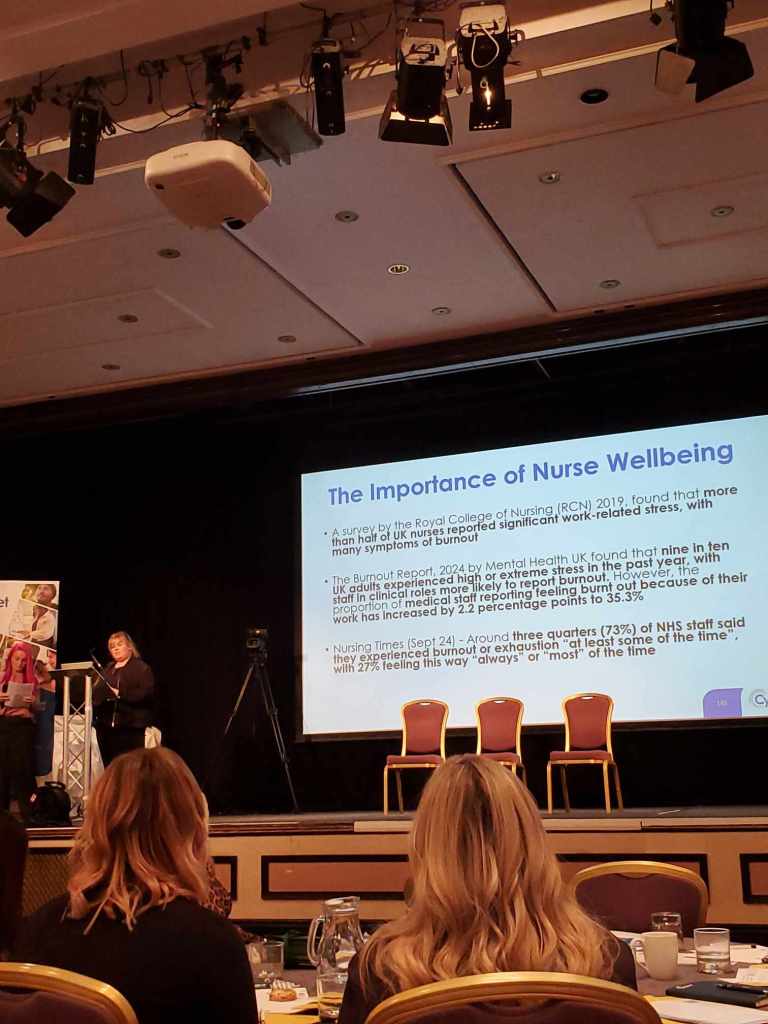
14:15 – Keynote: Nurse Wellbeing
Ali Curtis & Kerry Matthews, Cygnet Group
Ali Curtis and Kerry Matthews gave a heartfelt, powerful presentation that really spoke to the carer in me. Their session wasn’t just about workplace wellbeing it was about creating a culture of care for those who care.
They highlighted the deep emotional load that nurses carry every day, and how that weight is often invisible until it breaks someone. As a carer, I’ve seen the difference a compassionate nurse can make how their patience and presence can calm my loved one in a moment of crisis. But I’ve also seen the toll it takes on them. This talk brought that reality into the spotlight with honesty and respect.
What really struck me was the emphasis on psychological safety and holistic wellbeing. Kerry spoke about initiatives such as trauma-informed support, peer-to-peer networks, and dedicated wellbeing spaces—not just as nice add-ons, but as essentials for a safe and thriving workforce. It made me reflect: if we expect nurses to show up fully for our families, then we must show up for them too.
Ali touched on the importance of compassionate leadership—how leaders who listen, value staff voices, and lead with kindness set the tone for entire teams. This wasn’t just theory; it was grounded in real, measurable action being taken across Cygnet. Their Wellbeing Month, engagement surveys, and direct responses to staff feedback showed a commitment to continuous improvement.
14:30 – Breakout Sessions
Personality Disorder Management – Dr. Mark Luffingham
Research in Health & Social Care – Caroline Harris-Birtles (I attended this one)

Caroline Harris-Birtles delivered a session that was both inspiring and demystifying. As a carer, research can sometimes feel like a distant concept something that happens in universities, not in the everyday lives of those supporting someone with complex health needs. But Caroline brought it down to earth.
She spoke passionately about making research more accessible and embedded in practice. What stood out most to me was her commitment to involving people at every level clinicians, support staff, and crucially, people with lived experience. Caroline emphasised that research doesn’t always need to be academic or published to be meaningful; even small, practice-based projects can lead to real change in how care is delivered.
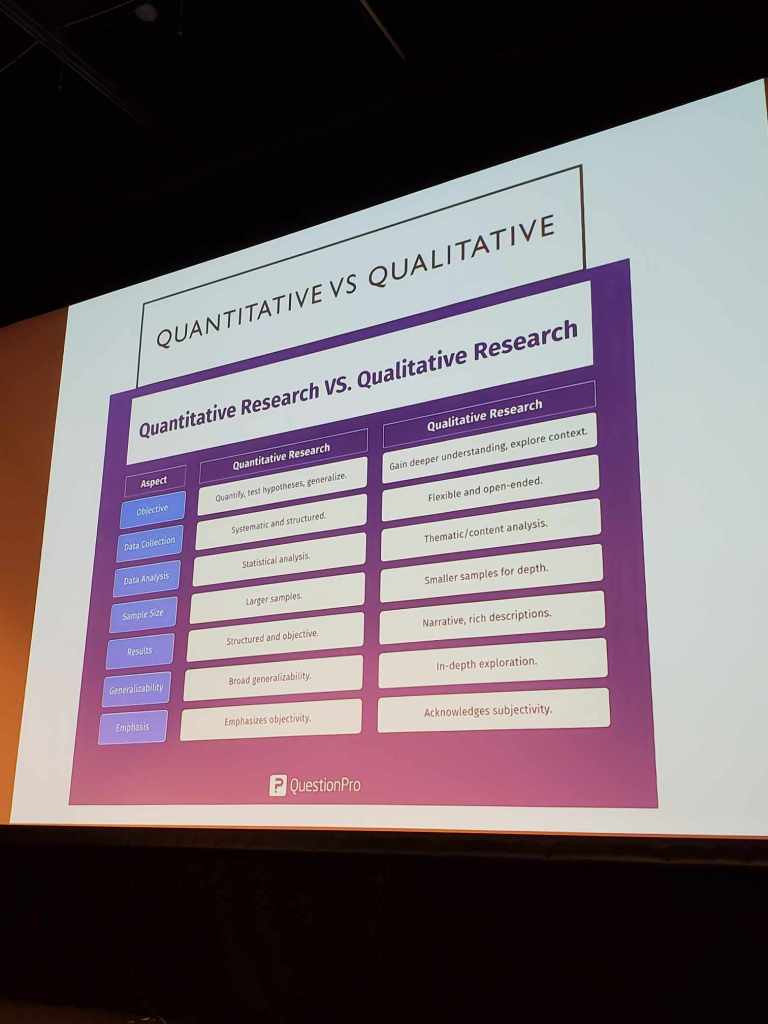
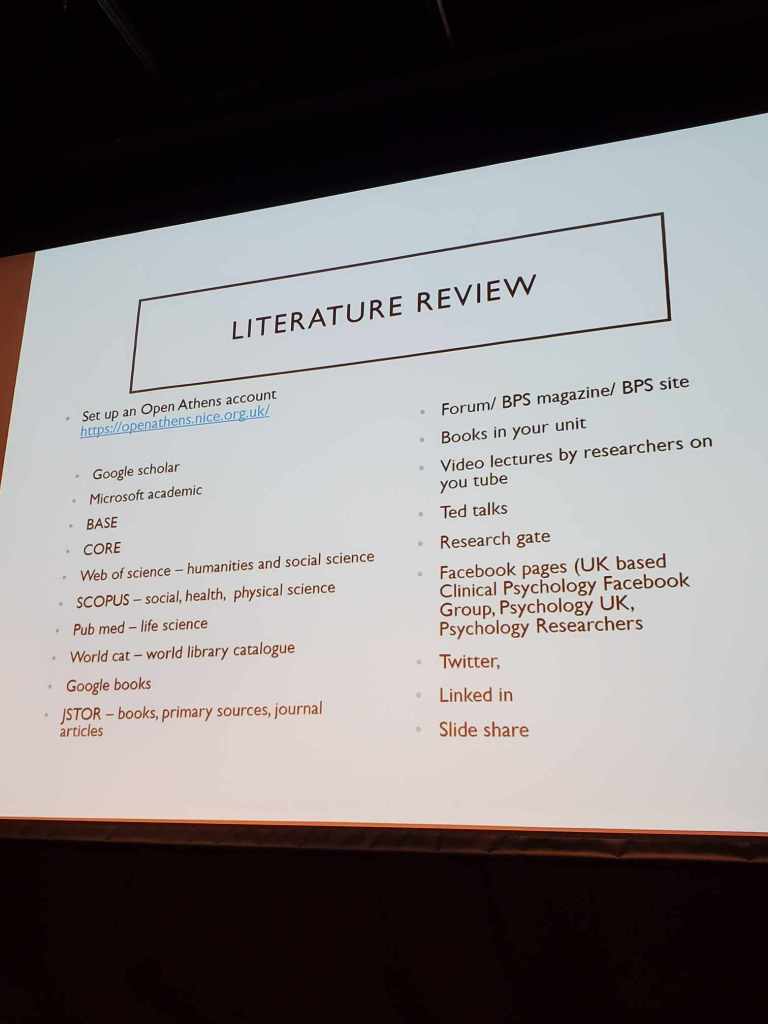
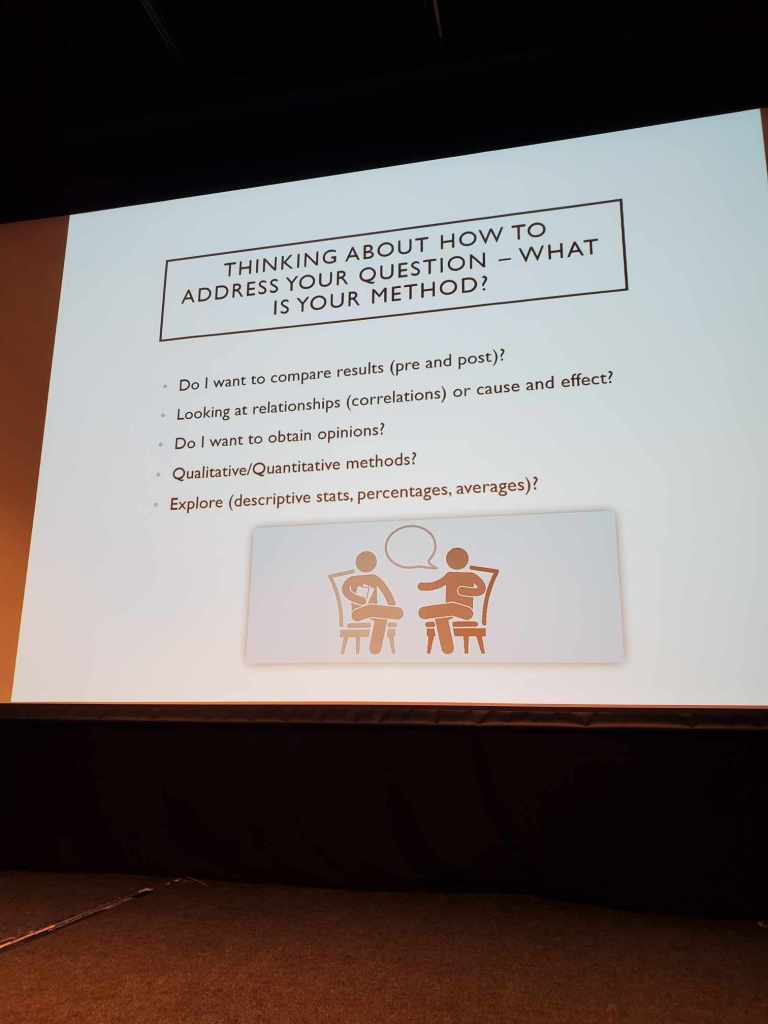
Her talk also highlighted common barriers to engaging in research, like lack of time, confidence, or support, but she didn’t just name them, she offered solutions. Resources, guidance, and a shift in mindset were part of her call to action: that anyone in the system can ask questions, explore problems, and find evidence-based ways to improve things.
For me, this session reinforced the importance of co-production. Caroline’s inclusive approach echoed the values we hold dear as carers: that the best outcomes come when people are heard, involved, and respected in shaping services. Her talk felt like an invitation not just to nurses and healthcare professionals, but to carers and service users to be part of creating better, kinder, more effective support.
Management of Epilepsy – Vickie Peters
15:30 – Cygnet Nursing Awards 2025 & Graduation Ceremony













As the awards portion of the day unfolded, I witnessed recognition of compassionate leadership, trauma-informed approaches, and those who had gone above and beyond. The message was clear: You are seen.
The awards and graduation ceremony marked a truly emotional high point of the conference. As a carer ambassador, witnessing the recognition of nurses and healthcare professionals who go above and beyond every day was affirming. These are the people we trust with the wellbeing of our loved ones and seeing their hard work publicly acknowledged felt incredibly personal.
The ceremony celebrated not only those completing their training and development pathways but also those who had demonstrated exceptional leadership, compassion, inclusion, innovation, and resilience. Names like Jerome Omesa, Sheila Muchenje, Josie Tate, and Zoe Koltman stood out as examples of what person-centred care looks like in action.
One speaker reminded us: “We must address our own wellbeing with the same professionalism we apply to others.” As carers, that felt like a quiet revolution. A reminder that we, too, are worthy of care.
16:25 – Closing Remarks (was done earlier in the day)
Dr. Tony Romero, CEO, Cygnet Group
Dr. Romero’s words created a bridge. His address wasn’t just about strategy or statistics; it was about human connection, pride in nursing, and the centrality of care.
He acknowledged the difficult years behind us and the pressures that nurses and care teams continue to face. But more importantly, he reinforced a vision for the future—one that positions nurses as leaders, innovators, and the heart of service transformation. His commitment to listening to staff, empowering them to drive change, and anchoring decisions in values felt sincere.
Dr. Romero also spoke directly to the impact nurses have on individuals and families, something I appreciated deeply. He reminded everyone in the room that care is not a transaction it’s a relationship. And when we get it right, the ripple effects change lives.
Themes That Truly Mattered as a Carer Ambassador
🔷 “Nurse Wellbeing” is Everyone’s Wellbeing
The conference theme wasn’t a slogan it was foundational. If nurses are supported, resourced, and cared for, that compassion reaches the bedsides, carers, and communities they serve.
🔷 Valuing Lived Experience in Leadership
Multiple speakers emphasized lived experience roles, not just for token inclusion but as essential to strategy, training, and accountability. It gave me hope to see peers in decision-making rooms.
🔷 From Triangle of Care and PCREF to Action
Whether through monthly engagement meetings or better carer engagement, organisations are waking up to the unmet need of carer inclusion and putting plans into place.
Thanks for reading…..till next time!