Welcome back to a brief update of the National Triangle of Care Commnity Group. A meeting organised by myself as a carer of lived experience to give a chance for mental health carers to find out developments on Triangle of Care. The online group is attended by unpaid mental health carers, Carers Trust triangle of Care leads and NHS carer representatives and mental health staff.
Agenda of Meeting
The meeting focused on discussing the Triangle of Care program, gathering feedback from carers, and addressing challenges in mental health care. Attendees shared experiences and insights on carer involvement, communication issues, and the need for improved support systems. Key topics included progress updates on the Triangle of Care implementation, the importance of carer perspectives in healthcare decision-making, and strategies to enhance carer engagement and representation across diverse groups.

Triangle of Care Program Updates
As the meeting organizer, I welcomed everyone and introduced the purpose of the meeting, which was to discuss the Triangle of Care program and gather feedback from carers. I mentioned at the meeting I would present feedback from challenges I hear from carers on the Triangle of Care program. Debbie and Mary, who are co-leads for the Triangle of Care program at Carers Trust, were also present to provide updates and answer questions. The meeting also included introductions from various participants, including carers and representatives from different organizations. The conversation ended with Debbie and Mary preparing to share some slides with the group.
Carers Trust Progress and Plans
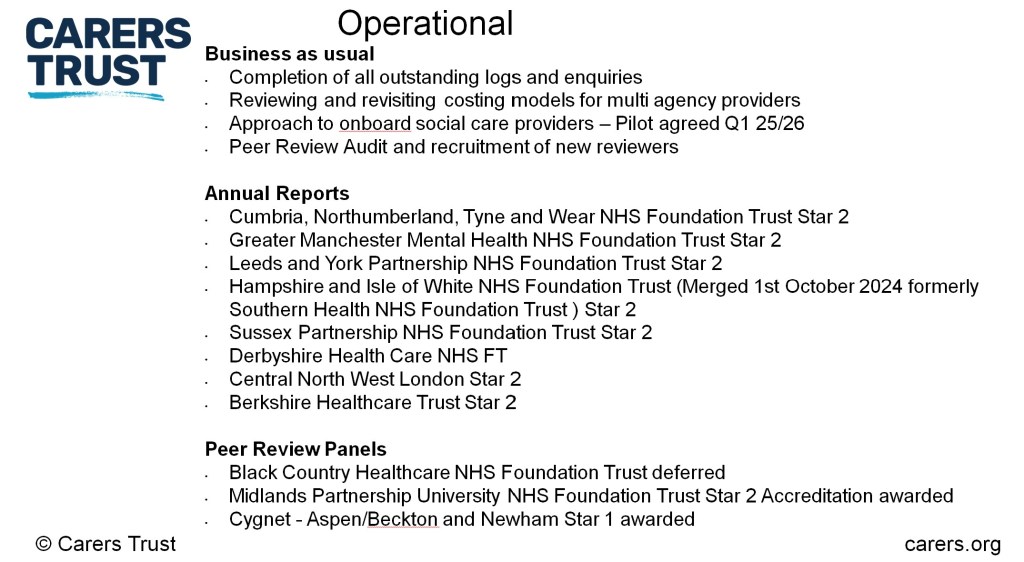
Debbie Hustings discussed the progress and future plans of the Carers Trust. She highlighted the work done in quarter 3, including the benchmarking and auditing of mental health members, managing expressions of interest, and the due diligence process.
She also mentioned the development of a community of practice and the use of digital auditing tools.
Plus receiving Triangle of Care updates and reports from the following NHS organisations. (click on picture below)
There are also annual reports and updates due from the following organisations below. The picture also shows the list of NHS MH trusts and private provider hospitals “Triangle of Care” Accreditions due.
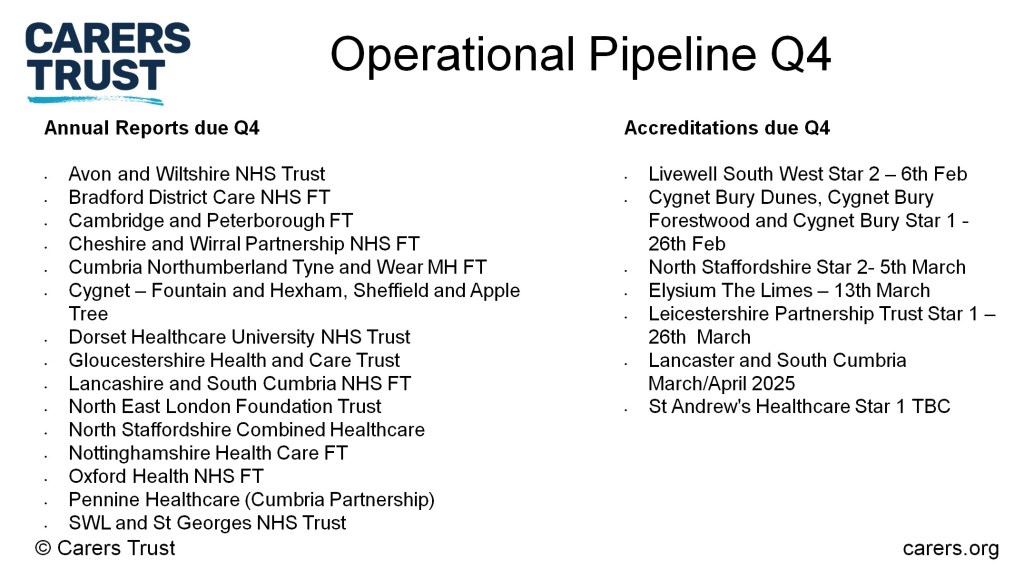
In quarter 4, they plan to onboard new providers, including Elysium, North Staffordshire, and Leicestershire, Lancashire, and South Cumbria. Debbie also discussed the engagement work, including the recruitment of new carers to peer review panels and the launch of a community of practice. Debbie mentioned the ongoing work on the social care pilot and the patient and carer race equality framework. The conversation ended with plans to standardize reporting templates and conduct a member survey to gather feedback.
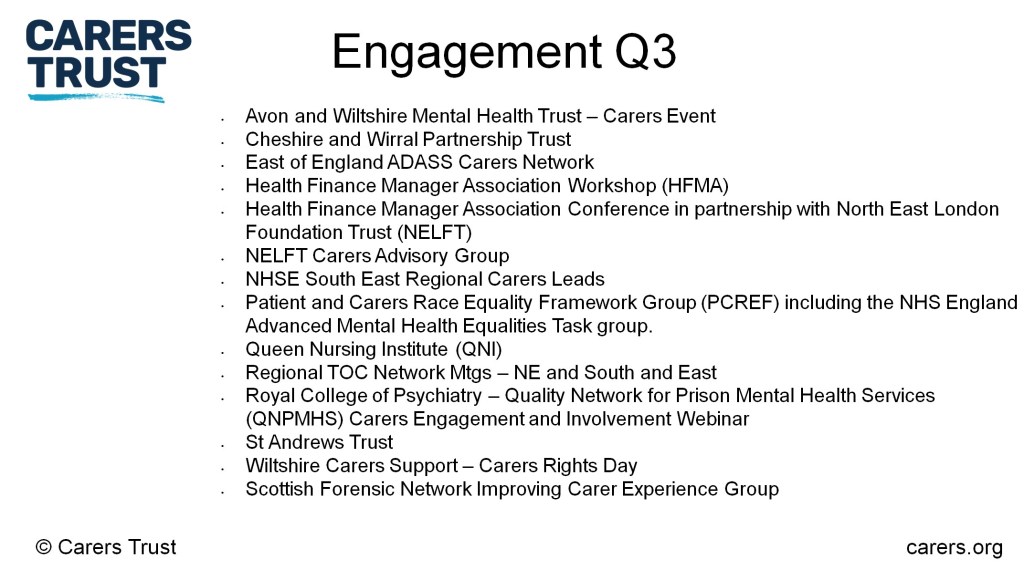
Carers Trust Triangle of Care leads reported that they have been working very hard on engagement, which I have included the list from the picture below.
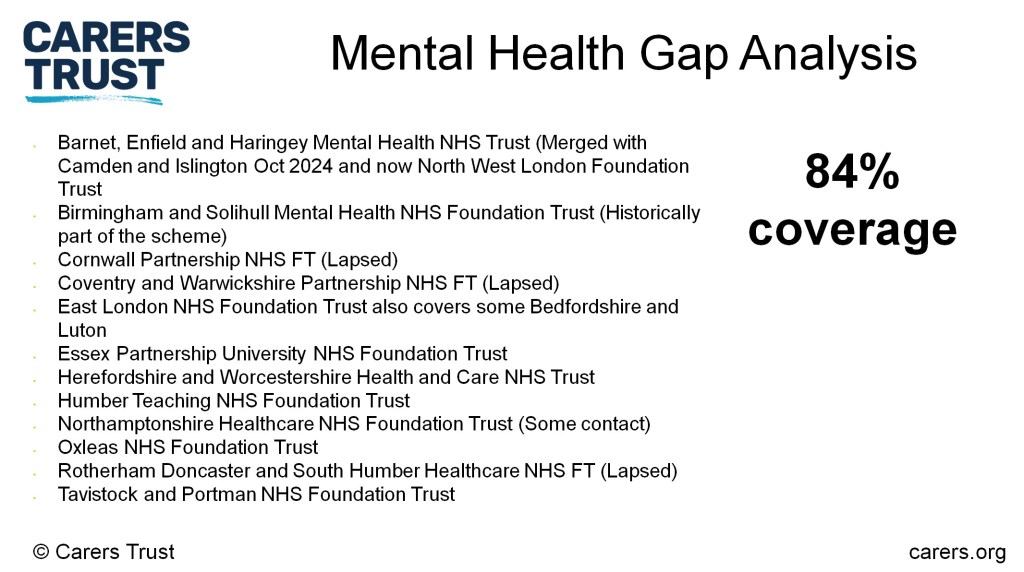
The Triangle of Care program is growing from strength to strength as shown from the picture below, we have 84% coverage. The list below shows organisations developing interest or looking to restart the Triangle of Care Program.
Triangle of Care Discussion
Debbie Hustings and myself initiated a discussion about the Triangle of Care, a framework for supporting carers. Amanda Cummins, Deputy Head of Coproduction Involvement at South West London and St. George’s, shared her insights on the current issues faced by carers, emphasizing the importance of communication, consistency, and confidentiality.

Amanda Cummins also highlighted the growing need for support around neurodiversity, particularly autism and ADHD. Amanda’s presentation was well-received, with several attendees sharing their personal experiences and expressing interest in the topic. Carers in attendance also shared their experiences with the Triangle of Care, highlighting its success in improving communication between staff and carers. The conversation ended with a discussion on the need for ongoing support and understanding of the issues faced by carers.
Concerns Over Direct Service User Contact
A carer in attendance also expressed concerns about the increasing trend of decision makers wanting to speak directly to service users, rather than carers, in mental health discussions. The carer felt this approach was counterproductive to the therapeutic relationship and the principles of the triangle of care. Amanda-Cummins agreed, attributing the issue to a lack of effective recording and monitoring of carer contacts in systems. She suggested that if carers were recorded and acknowledged, they would receive better support. The team also discussed the challenges of involving carers in strategic decision-making at Integrated Care Boards and the need for better education on the therapeutic relationship and the triangle of care. Alan Worthington founder of the Triangle of Care program raised the issue of carer burden and the need for more specialized autism nurses to address waiting lists and improve support for young people with autism.
Improving Healthcare Communication and Respect
In the meeting, Alan shared his experience with an elderly psychiatrist who effectively managed his twins’ serious illness by engaging with the family. He emphasized the importance of respecting the carer while also understanding the patient’s story. Amanda-Cummins and Alan discussed the need for better communication and respect in healthcare settings. DebbieHustings then discussed the work of the National Steering Group, emphasizing the need to align the Triangle of Care with the model of delivering racial equality for provider trusts. She also mentioned the plan to develop an evidence base for racial equality around the triangle of care. A carer of an ethnic background raised questions about the monitoring of equality, respect, and empathy in healthcare settings, to which Debbie responded by explaining the ongoing work with providers. Finally, I emphasized the importance of learning from each other and involving carers from diverse backgrounds
Addressing Carer Group Engagement Challenges
I then moved on to discuss the challenges faced by carer groups in engaging with trusts and the need for dedicated resources. I highlighted the issue regarding the challenges of tokenistic involvement and the need for genuine participation in shaping mental health care. I then moved on to mention the importance of carers’ voices being heard and the need for NHS trusts to combat these issues. Debbie Hustings suggested that the discussion could be stimulated further to encourage more input from the attendees.
Challenges and Progress in Carer Work
Debbie Hustings acknowledged the challenges faced by organizations in delivering the Triangle of Care model, emphasizing that it is a journey and not a static process. She highlighted the importance of annual reports to demonstrate continued progress and the need for dedicated resources to support carer work. Debbie also noted the diminishing funding for carer work and the need for a national drive to reinstate carers in policy terms. She expressed appreciation for the efforts of providers in challenging environments and encouraged them to continue their work.
Carer Leads and Support Collaboration
Debbie Hustings discussed the challenges faced by carer leads, emphasizing the need for support and collaboration. Tarek, the carer’s lead in Nelft, shared his experiences and the benefits of the Triangle Care format, which has helped reduce his isolation and provided a platform for sharing challenges and opportunities.

Alan suggested the role of leads in mobilizing care activity, creating ginger groups, and using ambassadors to establish relationships. He also proposed a competition to identify the trust with the most successful reduction in the duration of unrecognized caring. The conversation ended with me moving on to the next topic.
Integrating Carer Perspectives in Care
I then discussed the challenges of integrating carer perspectives into mental health care, including stigma, misunderstanding, and resistance to the culture change that the Triangle of care program is trying to provide. I highlighted the need for a balance between confidentiality and carer involvement in care planning. Debbie agreed with the points I raised, she then emphasized the importance of addressing these issues to support the evolution of the triangle of care. She suggested that the Carers Trust could facilitate more engagement between carer leads to reduce their isolation. Tarek added that there is a need for clinicians to think outside the box and consider the role of family in their clinical thinking.
Addressing Carer Engagement Challenges
The meeting discussed practical challenges in involving and supporting carers of mental health patients. I highlighted the lack of training for healthcare staff on carer engagement and awareness, leading to communication breakdowns. Carers themselves may face burnout and fatigue, limiting their ability to advocate effectively. Time constraints and misaligned schedules between carers and healthcare providers also pose challenges to getting feedback on services. Additionally, there are representation gaps, with voices of minority ethnic groups (ongoing development), young carers, and marginalized backgrounds being underrepresented. Debbie kindly acknowledged these issues and emphasized the need for empowering staff through carer awareness training, reducing consultation burden on carers, exploring innovative engagement methods like virtual meetings, and sharing best practices across providers. Key recommendations included consistent carer awareness training for staff, providing respite opportunities and well-being support for carers, fostering open communication and trust, allocating dedicated resources for carer initiatives, and promoting inclusion of diverse carer voices.