On May 1st, 2025, Cygnet Health Care hosted its landmark Co-Production in Commissioning Conference at the iconic Villa Park, Birmingham. More than just a professional gathering, the event was a manifesto for a more inclusive, compassionate, and equitable model of care, driven by people with lived experience, carers, clinicians, and commissioners alike.

Packed with powerful keynotes, practical models, and heartfelt stories, the day was as emotionally resonant as it was strategically focused.
- Opening the Day: A Full Room, A Clear Mission
The day opened with Cygnet’s leadership acknowledging the scope of the challenge ahead. With over 50 experts by experience now embedded across Cygnet hospitals, the organization signalled its intent to not only implement co-production, but lead on it nationally.
Raf Hamaiazia co-chair of Cygnet’s co-production programme emphasized that co-production is not an add-on, but central to the way care should be delivered. He acknowledged that while the term is widely used, its implementation varies wildly, and this conference was about defining what real co-production looks like.
He introduced the day as an opportunity not just for presentations, but for mutual learning, networking, and challenging assumptions.
Stephen Firn OBE, Chief Executive of Healthcare at Cygnet, noted that the event being sold out was more than just a success, it was a sign of a growing appetite for authentic co-production.
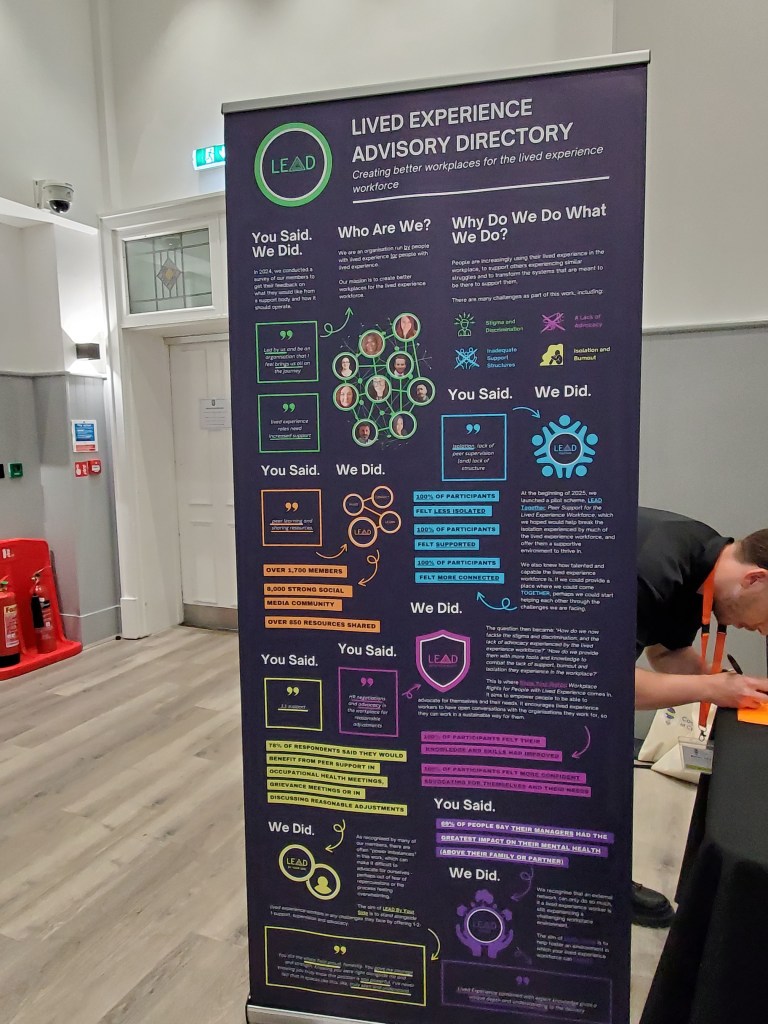
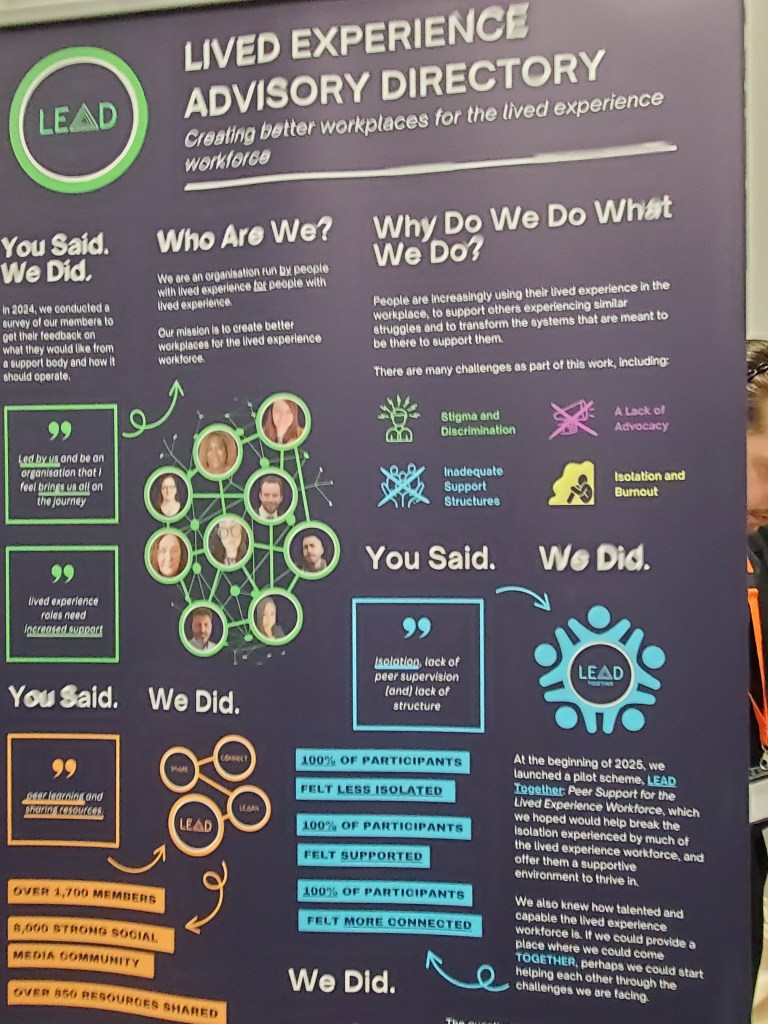
Delegates from organisations including Imroc, Lived Experience Advisory directory, the Design and Mental Health Network, Creative Football, and Rethink Mental illness joined by a broad coalition of service users, family carers, NHS commissioners, students, and policy shapers to network, share, and shift perspectives.





- Dr Geraldine Strathdee CBE, OBE: Power, Pain, and Possibility
Dr. Geraldine Strathdee’s talk was a powerful personal and professional reflection on leadership, mental health, and the transformative role of co-production and inclusive practice.
Personal Journey & Values
Geraldine began by reflecting on her upbringing in an excluded and impoverished community, shaped by conflict and disadvantage during the Troubles in Northern Ireland.
Her career path into psychiatry and leadership was rooted in a commitment to peace, equity, and social justice, inspired by local GPs and a belief that everyone has potential.
The Power of Belief and Human Potential
She emphasized that all people have skills and value, even when systems underestimate or overlook them.
Hope, respect, and belief are key tools in healing and empowerment, especially for those who’ve experienced trauma or marginalization.
Her message was clear: people are not problems to be fixed, but partners in creating solutions.
Co-Production and Multidisciplinary Collaboration
True co-production requires non-hierarchical, multi-agency working where services are designed with people, not for them.
She championed integrated teams that work across sectors to address not just mental health, but education, housing, substance use, and social relationships.
Inclusivity and adaptability are vital — services must meet people where they are, in their language, culture, and context.
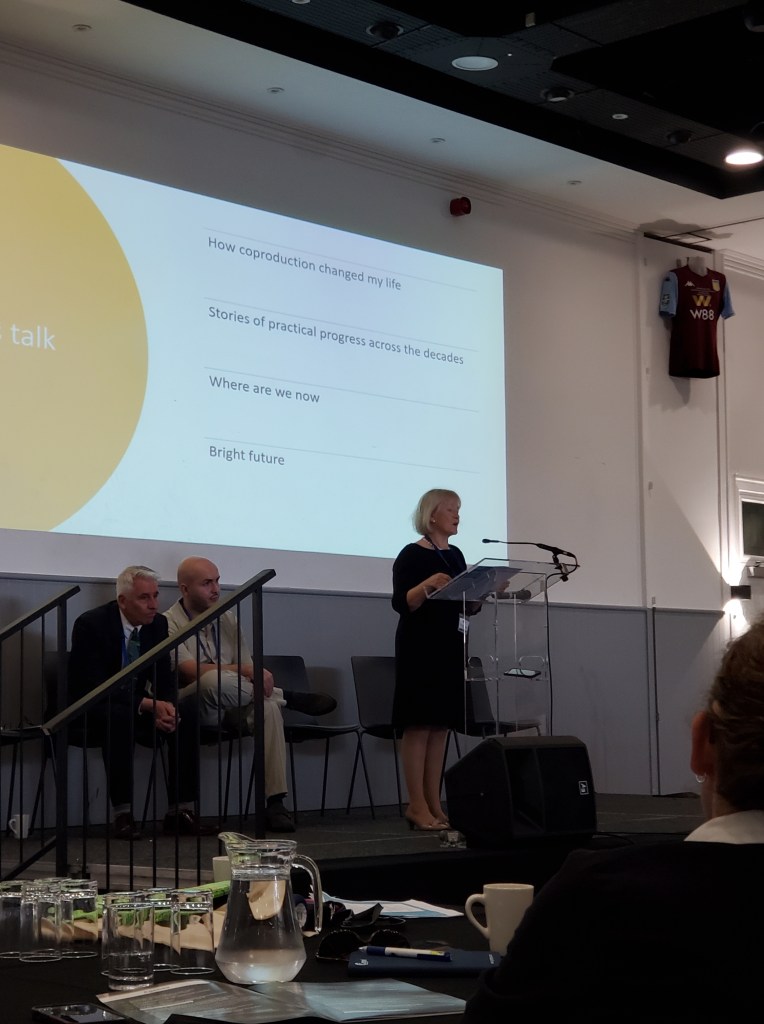
- Julie Repper, ImROC: Co-Production as Democracy
Dr. Julie Repper’s talk was a passionate and insightful argument for co-production as the foundation of meaningful, democratic, and inclusive health and social care systems.

Core Argument
Co-production isn’t optional or novel, it’s inevitable in modern services. The question isn’t whether it will happen, but how well it’s done. It’s about shifting power from professionals to communities and people with lived experience — to create more just, effective, and human-centered services.
What Is Co-Production?
- True co-production means involving everyone in decisions: professionals, service users, carers, and community members.
- It’s not just listening it’s sharing power, shaping services together, and ensuring that all contributions are equally valued.
- Co-production recognizes that lived experience is expertise — as valid as professional or academic knowledge
Doing It Right
- Avoid tokenism: It’s not about filling a seat at a meeting. It’s about real influence.
- Design with, not for: Don’t pre-decide the agenda. Let ideas come from the community.
- Adjust formats for accessibility, not everyone will sit in formal meetings. Meet people where they are.
- Geoff Brennan & Ali Curtis: SafeWards & Chameleon in Action
Geoff Brennan and Ali Curtis presented two co-production frameworks making measurable change in Cygnet’s services:
SafeWards:
A practical model to reduce conflict and coercion on inpatient wards
Uses discharge messages, mutual expectations boards, and positive words interventions
All co-designed with patients, ensuring real-time emotional safety.
Ali also stated on stage that Laura had informed her that she was a young carer, I felt that even though Ali is a professional, the statement was powerful as she had to be informed she was a carer. Ali’s passion to ensure carers voices are heard is evident in her work.
Chameleon (CAMHS):
Built for and by young people using inpatient services
Includes personal staff boards, co-designed murals, and structured community meetings with roles like “Chocolate Distributor”
Ensures co-production continues post-accreditation through peer review and champion-led action groups
One quote stood out:
“If the care relationships aren’t right, nothing else will work.”
After some panel discussions we broke for lunch and more networking, where I took the chance to visit some stalls.





Co-Production in Social Care – Real Voices, Real Homes
Speakers: Ollie White, Ryan Hartnett, and Jonathan
Organisation: Cygnet’s Social Care Division
This powerful session explored how co-production in residential care homes is not only possible, but transformative. The speakers, including Jonathan, a resident and quality guardian, gave personal, on-the-ground insight into what real inclusion looks like in social care environments.
While much of the conference focused on healthcare settings, Ollie, Ryan, and Jonathan reminded the audience that residential care brings different challenges—and therefore, requires different co-production approaches.
“What works in a hospital won’t always work in a home—but the need to be heard is the same.”
There was an explanation on how the Quality Guardian programme gives residents the opportunity to:
- Conduct peer-to-peer reviews of other homes
- Provide structured feedback on food, activities, environments, and staff relationships
- Help management teams reflect and act on real-time insight
- Identify what really matters to the people living in services—beyond compliance and paperwork
- This isn’t symbolic input. It’s embedded influence—and it’s helping services improve meaningfully and consistently.
- Julian De Takats – Reclaiming the Triangle of Care: Carers as Co-Producers
Julian De Takats delivered one of the most personal and passionate presentations of the day representing Cygnet’s Carers Network.
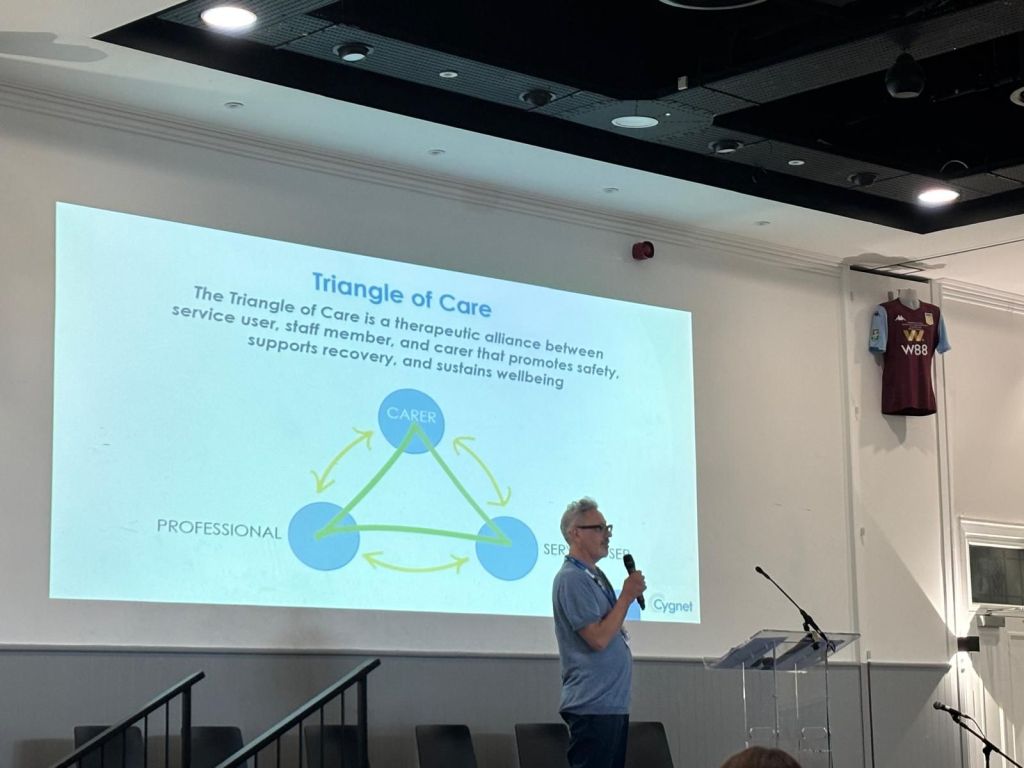
Julian focused on the Triangle of Care, a model that promotes a therapeutic alliance between the service user, the professional, and the carer.
Framing carers as a neglected but vital group of lived experience contributors, Julian advocated for their systematic inclusion in care and decision-making.
“We often talk about experts by experience, but carers are also lived experience experts. Partners, siblings, parents our insight matters.”
Julian’s talk was grounded in personal experience. It took him eight years into his son’s mental health journey before anyone formally acknowledged him as a carer. That moment of recognition, he explained, marked the start of his own co-production journey.
The Six Standards of the Triangle of Care
Julian walked through each of the six standards of the Triangle of Care, showing how Cygnet is working to co-produce them with carers:
- Carer Identification
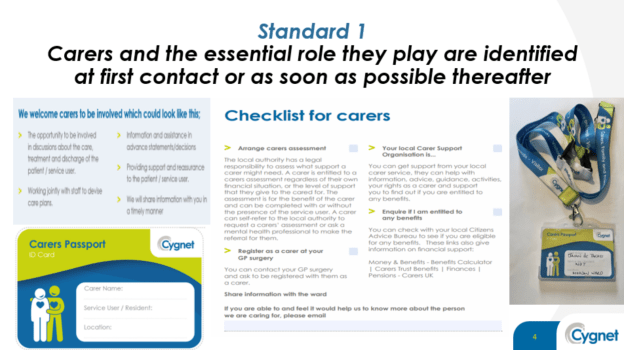
Many carers don’t know they are carers. Julian shared that he only discovered his role when invited to a carer event—highlighting the need for early, proactive identification.
- Carer Involvement in Care Planning
Co-producing partnership agreements to define how often carers want to be contacted and how they wish to contribute.
- Staff Training & Awareness

Carer awareness training, co-designed and co-delivered by carers, is now embedded into Cygnet’s induction process.
Training includes lived experience videos and regular masterclasses hosted by carer ambassadors.
- Information Sharing & Consent
Julian tackled the complex issue of consent head-on. He described a co-produced roundtable that redesigned consent forms to avoid the outdated “we can’t tell you anything” barrier.
The goal: balance privacy with compassion and communication.
- Carer Leads and Champions

He stressed the need for clear roles in services—carer champions who offer support, answer questions, and ask, “How are you?”
- Support and Information
Julian discussed how Cygnet co-produced plain-language booklets, replacing acronym-heavy guides that alienated families.
Carer feedback surveys and notice boards have also been shaped with input from carers, ensuring relevance and accessibility.
Julian emphasised how emotional impact, storytelling, and real engagement can change mindsets. He credited Laura Sheridan, a key colleague and fellow carer, for encouraging him to channel frustration into advocacy. Together, they co-produced much of the carer-facing material now in use across Cygnet.
- Nick Hunter – Co-Producing Better Physical Health in Secure Care
Nick opened with a powerful reflection on his personal lived experience as someone who spent time in secure care. He shared how severe side effects from medication, poor diet, and a lack of physical activity during his admission had long-term health consequences—including weight gain, high cholesterol, and emotional distress.
“It was predictable and avoidable—but it happened. And it still happens.”
He stressed that physical health in secure settings is too often neglected, despite strong national guidance. This results in preventable illness, early mortality, and significant distress for individuals and their families.
- Lived Experience as a Driver for Change
Nick’s new role is part of a progressive shift: using lived experience to inform commissioning. He is helping develop strategies that are both practically effective and personally meaningful to those in secure services.
Nick presented sobering statistics:
- People in secure settings face much higher rates of chronic illnesses, including heart disease, diabetes, cancer, and liver disease
- Many die 15–20 years earlier than the general population
- These deaths are largely preventable, linked to diet, exercise, smoking, and poor access to routine care
- Strategic Action Plan
The collaborative is now implementing a structured, co-produced strategy that includes:
Annual physical health checks for all patients
A community of practice model to share learning and standardise care
A physical health steering group with lived experience at the core
New training pathways, including peer-led physical health awareness
- Environment and Staff Readiness
Nick noted that environments must support physical health through:
Better food choices
Active lifestyle opportunities
Staff training on how to support people with complex needs (including older adults, neurodivergent individuals, etc.)
Next we had a song by Tasha called “Superwoman” is a heartfelt, emotional ballad that reflects on pain, resilience, and inner strength.
Attending Cygnet’s Co-Production in Commissioning Conference 2025 was both inspiring and enlightening. I learned that true co-production is not just consultation. it’s about power-sharing, inclusion, and equity. The event demonstrated how co-production can transform care when it’s practiced with authenticity, not tokenism. From Dr. Geraldine Strathdee’s deeply personal insights on leadership and human potential, to Dr. Julie Repper’s argument that co-production is a democratic necessity, every speaker reinforced the value of lived experience in shaping services. I saw practical examples like SafeWards and the Triangle of Care come to life, where service users, carers, and professionals worked as equal partners to improve outcomes. The conference was well planned, emotionally powerful, and meaningfully involving. It left me convinced that co-production is not only the right way to work it’s the only way to build compassionate, effective, and future-ready services.