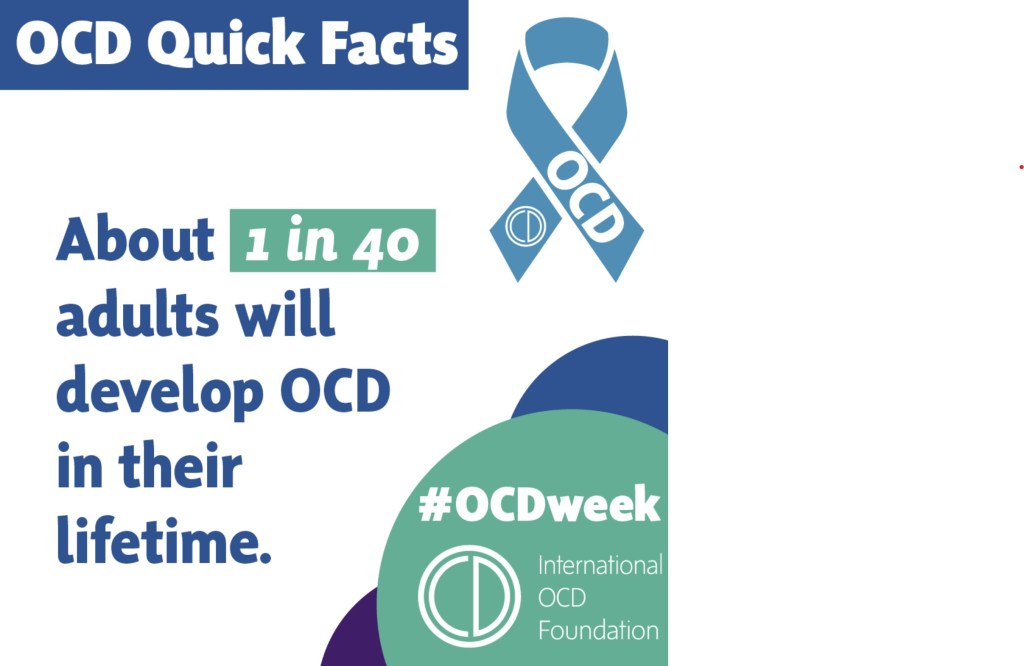
Welcome back to another mental health awareness blog post from carer activist Matthew McKenzie. As of the posting of this blog. It is OCD Awareness Week 2024. You can also watch my video of the awareness week below.
What is OCD?
Obsessive-Compulsive Disorder (OCD) is a mental health condition that affects millions of people worldwide. It involves unwanted, intrusive thoughts known as obsessions and repetitive behaviors or mental acts called compulsions. These behaviors are not just quirky habits but are driven by a deep need to alleviate the anxiety caused by these intrusive thoughts.

Understanding the Obsessions
Obsessions are more than just everyday worries or concerns. They are persistent and unwanted thoughts, images, or urges that cause significant anxiety or distress. People with OCD are often fully aware that these thoughts are irrational, but they find it extremely difficult to ignore or suppress them.
The Nature of Compulsions
Compulsions are repetitive behaviors or mental acts that a person with OCD feels driven to perform. These actions are attempts to reduce the distress caused by obsessions or to prevent a feared event or situation. Compulsions can take many forms, including excessive hand-washing, checking, counting, or repeating words silently. Importantly, these behaviors usually provide only temporary relief and can be very time-consuming, interfering significantly with daily life.
Busting Myths About OCD
It’s Not Just About Tidiness
One of the most common misconceptions is that OCD is merely about being neat and organized. While some people with OCD may have cleanliness-related compulsions, the disorder is much more complex. It can involve a wide range of obsessions and compulsions, many of which have nothing to do with order or cleanliness.
Beyond Quirks and Idiosyncrasies
OCD is often trivialized in popular culture as just a set of quirky behaviors. In reality, it is a serious condition that can cause significant distress and impairment in various areas of life, including personal relationships, work, and overall well-being.
The Role of OCD Awareness Week 2024

Organized by International OCD Foundation
This year’s OCD Awareness Week, running from October 13th to the 19th, is being spearheaded by the International OCD Foundation and other reputable organizations. The main goal is to spread awareness, break down stigma, and provide actionable support for those living with OCD.
Activities and Resources
The week will feature various workshops, webinars, and support groups designed to educate the public and those affected by OCD. Educational materials and personal stories will also flood social media, providing a wealth of knowledge and resources. Keep an eye on hashtags like #OCDWeek to stay updated on these activities.
How You Can Help
Educate Yourself
If are caring for someone with OCD, taking the time to educate yourself about their condition can be a game-changer. Understanding their symptoms, knowing their triggers, and familiarizing yourself with treatment options can make you a better support system for them.
Combat Stigmatization
One of the critical goals of OCD Awareness Week is addressing common misconceptions and combating stereotypes. Recognize that OCD is not something to be joked about—it is a serious condition that requires empathy and understanding.
Effective Treatment Options
Cognitive Behavioral Therapy (CBT)
Cognitive Behavioral Therapy (CBT) is one of the most effective treatments for OCD. This type of therapy involves techniques to help individuals manage their obsessions and reduce compulsive behaviors. One specialized form of CBT, called Exposure and Response Prevention (ERP), is particularly effective for treating OCD.
Medication
Medicinal interventions, particularly selective serotonin reuptake inhibitors (SSRIs), can also be very effective in managing OCD symptoms. It’s essential to consult a healthcare professional to determine the best treatment plan for each individual.
Seeking Professional Help
It’s crucial to know that help is available and that it’s okay to seek it. Professional treatment can make a significant difference in managing OCD symptoms and improving quality of life.
Building a Supportive Community
The Power of Empathy
One of the most impactful ways to support those living with OCD is through empathy and understanding. Small acts of kindness, like listening without judgment or offering a helping hand, can go a long way in making someone feel less isolated in their struggle.
Family and Friends
Families and friends play a crucial role in the support system for someone with OCD. By educating themselves about the disorder, they can offer better support and reduce the feelings of isolation and stigma that often accompany mental health conditions.
Get Involved
Spread the Word
Sharing knowledge is one of the simplest yet most effective ways to raise awareness. Use social media, community events, and even casual conversations to spread accurate information about OCD. Participate in events and activities during OCD Awareness Week to show your support.
Promote Compassion
By promoting empathy and understanding, we can create a more compassionate world for those affected by OCD. Every small effort counts, from sharing a post on social media to participating in a local awareness event.
Making a Difference
Raising awareness about OCD is not just about understanding the condition but also about fostering a supportive environment for those affected. By debunking myths, spreading correct information, and showing empathy, we can make a transformative impact in the lives of millions of people living with OCD.
Thank you for taking the time to learn about OCD and how you can contribute to raising awareness. Let’s make this world a little more compassionate and understanding, one step at a time.