Another blog post from Matthew McKenzie carer activist and author of “Experiencing mental health caregiving”. Here in this blog, I discuss about how caring for someone with mental illness can be overwhelming to navigate through the various services and professionals involved.
Knowing who to contact and when can make a significant difference in the effectiveness of the care provided. In this article, we delve into the key staff members that are typically involved in a community mental health team and the roles they play.
If you want to watch the long view video (27 minutes). Please click the video blow
The Core Team Members
Psychiatrists

Psychiatrists are often the cornerstone of a mental health team. These medical doctors specialize in diagnosing and treating mental health disorders. They are responsible for prescribing medication and developing care plans. As a carer, it is crucial to have a good relationship with the psychiatrist, as they play a pivotal role in the overall treatment plan of your loved one.
Psychologists
Psychologists focus on assessing and treating mental health issues through psychological therapies rather than medication. They provide various types of therapies and conduct tests to understand the patient’s mental state, helping them cope through recovery processes. While they do not prescribe medication, their role is vital in assisting with the psychological aspects of mental health.
Mental Health Nurses

These registered nurses have specialized training in mental health. They offer care and support, help manage medication, and often work directly with both patients and their families. Their presence isn’t limited to inpatient settings; they are also found in community settings, providing consistent and essential support.
Clinical Social Workers
Social workers in mental health settings provide therapy and support to both the individual and their family. They assist in accessing community resources, which are crucial once the patient moves out of institutional settings. They act as a bridge between the community and the mental health system, helping navigate through various social services.
Counsellors and Therapists

These professionals offer individual or group therapy, focusing on the emotional and psychological challenges faced by the patient. Their role is similar to that of psychologists but often focuses more on the practical aspect of dealing with daily mental health challenges.
Specialized Support
Occupational Therapists

Though less common, occupational therapists play a significant role by helping individuals develop, recover, and maintain daily living and work skills. They use therapeutic activities to achieve these goals, which are crucial for the patient’s integration into everyday life.
Psychiatric Technicians
These staff members assist with the day-to-day care of patients, especially in psychiatric facilities, and monitor behavior. Their role is mostly found in settings where the patient’s mental health condition requires intensive intervention.
Addiction Specialists
Addiction specialists are crucial for patients dealing with substance use disorders. They provide therapy and support, focusing specifically on recovery from addiction, which can be closely intertwined with other mental health conditions.
Rehabilitation Specialists
These professionals help patients with mental illnesses develop skills for independent living and integrate into the community. Their work is essential for long-term recovery and improving the quality of life for individuals with mental health issues.
Coordination and Crisis Management
Case Managers
Case managers, although rare, play a vital role when present. They help patients and their families navigate the mental health services, ensuring that necessary resources and supports are accessed. Their role often overlaps with that of clinical social workers or care coordinators.
Crisis Intervention Specialists

These trained professionals respond to mental health crises, providing immediate support and stabilization for individuals in distress. Their role is critical in emergencies, ensuring that the person gets the help they need promptly.
Family and Community Support
Family Therapists

Family therapists specialize in working with families to improve communication, resolve conflicts, and support individuals with mental ill health. Their role is crucial in ensuring that the family as a whole can cope with and support the patient effectively.
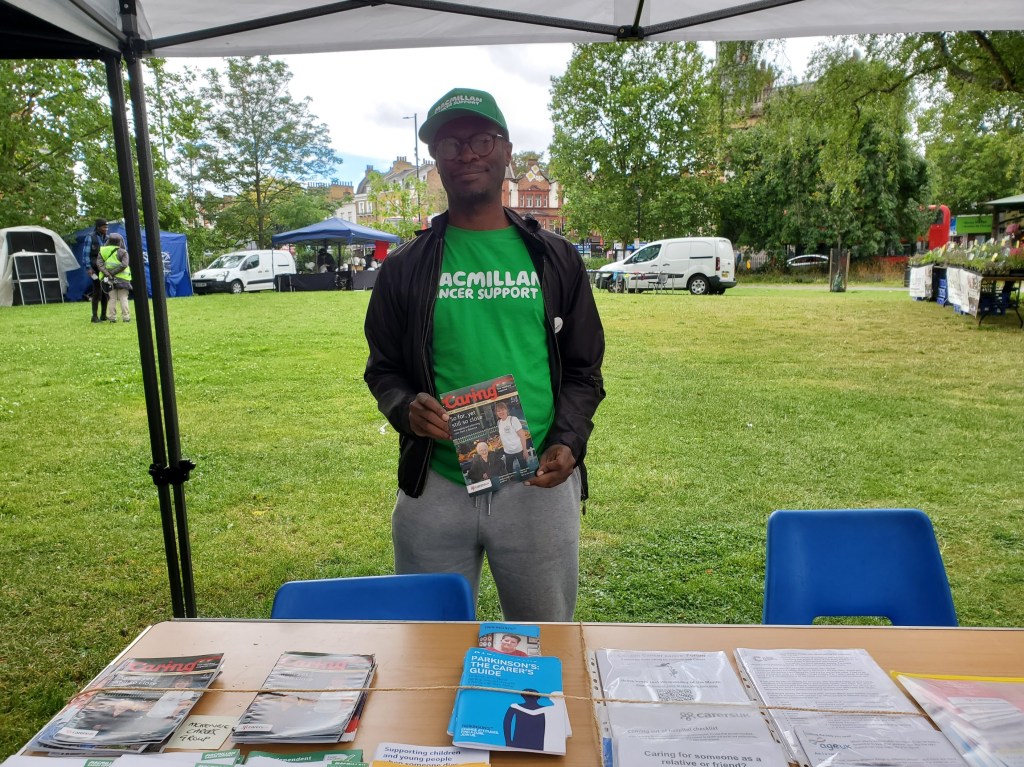
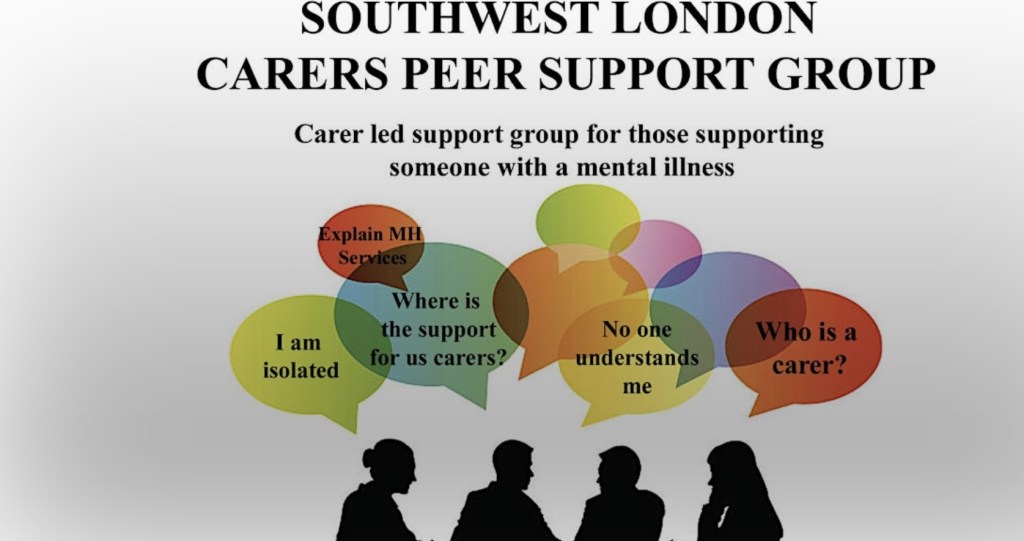
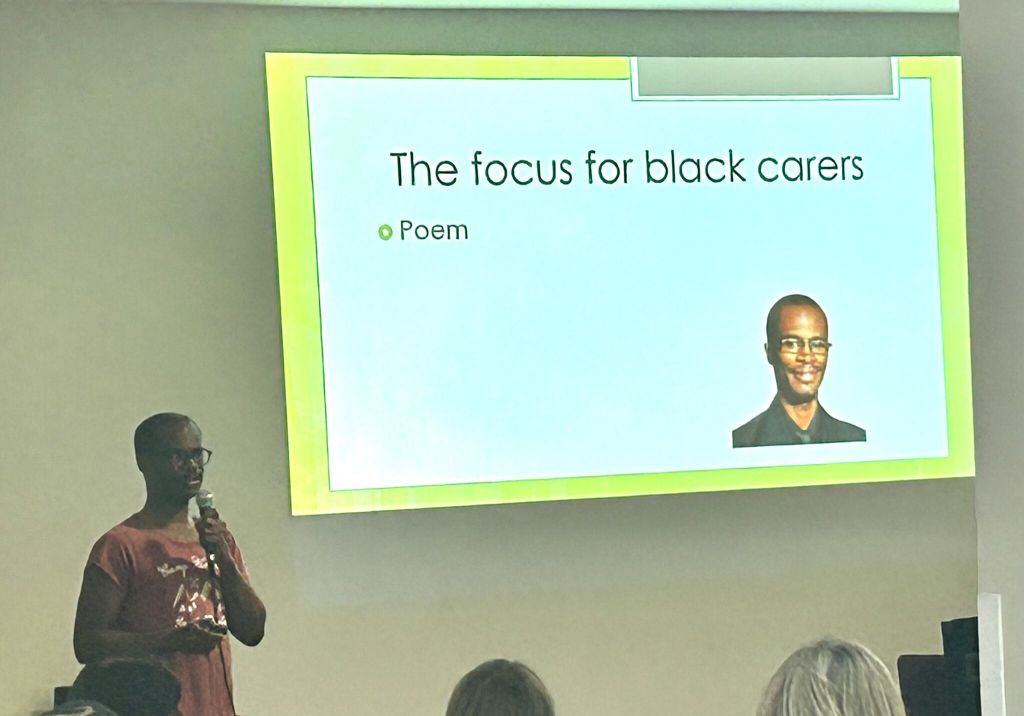
Peer Support Specialists
Peer support specialists use their lived experiences with mental health issues to provide support and guidance to others facing similar challenges. They offer hope and a unique form of empathy and understanding, making them a crucial part of the mental health team. Take note, not all peer support specialists are the same. Carer peer support specialists are a new trend, but will be a rare resource compared to mental health peer support.
Community Outreach Workers
These workers connect individuals and families with community resources and support services. They focus on prevention and education, ensuring that the patient and their carers know about and can access necessary supports.
Additional Roles
Administrative Staff

These are the personnel who handle scheduling, intake, and other administrative tasks. They ensure smooth operations and access to services, often being the first point of contact for carers seeking assistance.
Dieticians and Nutritionists

Mental health can significantly impact physical health, including nutrition. Dieticians and nutritionists specialize in addressing the nutritional needs of individuals with mental health issues, emphasizing the connection between diet and mental well-being.
Art and Music Therapists

Creative therapists use art and music as therapeutic tools to help individuals express emotions and process experiences. These therapies offer alternative ways to cope with mental health challenges, often as part of a broader treatment plan.
Community Outreach Workers
Staff who connect individuals and families with community resources and support services, often focusing on prevention and education.
Pharmacists
Pharmacists play an essential role in medication management, reviewing prescriptions, and advising on proper medication use. They collaborate closely with psychiatrists to ensure that the medication plan is effective and manageable for the patient.
Enhancing Collaborations

Understanding the roles within the community mental health team allows carers to better advocate for their loved ones. It leads to more effective communication and faster resolution of concerns. Building relationships with these team members facilitates a coordinated approach to care and treatment.
Accessing Resources
Identifying the right professionals can help carers access valuable resources and educational materials tailored to their situation. This is particularly important for long-term support and recovery.
The Importance of a Carer Support Officer

Among all the roles, care support officers are perhaps the most crucial for carers. They can act as the main link between the mental health staff and the carers, providing education, training, and support. They listen to carers, relay concerns, and remind them of their own well-being, sometimes even conducting carer assessments.
Conclusion
As a carer, familiarizing yourself with the mental health team can significantly enhance the support you provide to your loved one. Understanding who to contact for specific needs helps in effective navigation of the mental health system. The more you know about the team’s structure and roles, the better you can advocate for and support your loved one’s journey towards recovery.
Navigating the mental health system can be complex, but with the right knowledge and support, carers can make a significant difference in their loved one’s treatment and recovery process.