Welcome back to another blog post by carer activist Matthew McKenzie. I usually blog to help to educate unpaid carers on navigating health systems and strengthening their carer identity.
Today we are looking at why and how carers can escalate complaints if disatisfied about responses from health or social care services.

I have also done a video if you wish to see examples of complaints and escalations. (23 Minutes). Please click on the video below to watch.
As an unpaid carer you can learn how to navigate escalating complaints in unpaid care, from informal concerns to legal action and media attention. Empower yourself to advocate for quality care and address systemic failures effectively.
Introduction
Navigating the complexities of healthcare systems can be challenging, especially for unpaid carers who dedicate themselves to looking after a loved one struggling with long-term mental or physical health issues.

Often, situations may arise where the care being provided falls short of acceptable standards, compelling carers to lodge complaints. Unfortunately, not all carers are well-informed about how to escalate these complaints effectively. This blog provides a comprehensive guide to unpaid carers on escalating complaints in various stages, from initial informal resolutions to severe legal actions.

Understanding the Importance of Complaints
Before delving into the stages of complaint escalation, it’s crucial to understand why raising concerns and complaints is so important. Complaints serve multiple purposes—they highlight deficiencies in the system, enforce accountability, and, most importantly, ensure that the care recipient gets the best possible treatment. Carers must recognize that it’s their right to complain if the services provided do not meet acceptable standards.

Initial Steps for Complaints
Informal Concerns and Basic Level
The first step in resolving any issue should ideally be informal, characterized by direct and immediate communication with the professional involved. This could be a social worker, care coordinator, or any key member of the mental health team.

Preparing for the Meeting
Preparation is key to a successful resolution. Carers should come equipped with detailed notes, including dates and instances of lapses or failures. Bringing along the service user’s care plan can lend weight to the complaint and provide a concrete reference for the discussion. This method is most effective for minor issues such as delays in communication or minor discrepancies in the care plan.
Escalating to Written Complaints
Intermediate Level
If informal attempts do not yield satisfactory results, the next step is to submit a formal written complaint. This involves documenting all concerns, efforts made to resolve them, and any pertinent evidence.
You can also contact your local Healthwatch to feedback on services or get advice on the best way to complain.

Writing the Complaint
When writing the formal complaint, ensure to:
- Detail your concerns comprehensively
- Include records of prior communication attempts and failures
- Provide specific dates and names of the individuals involved
- Clearly state your desired outcome
Timeframes for Resolutions
Generally, service providers are required to acknowledge receipt of the complaint and provide a timeline for investigation, usually ranging from 20 to 40 working days, depending on the complexity of the issue.
Seeking Mediation and Further Assistance
Escalation to PALS or Advocacy Services
If the issue remains unresolved, carers can seek help from PALS (Patient Advice and Liaison Service) or advocacy services. These intermediate-level services can provide guidance, represent the complainant, and even escalate the complaint within the service provider’s framework.

Contacting PALS or Advocacy Services
PALS offers confidential advice and can work as intermediaries between the carer and the care team, helping to navigate the complaints process effectively. Advocacy services can assist in drafting the complaint and ensuring that all necessary documentation is in order.
Formal Regulatory Bodies
Advanced Level
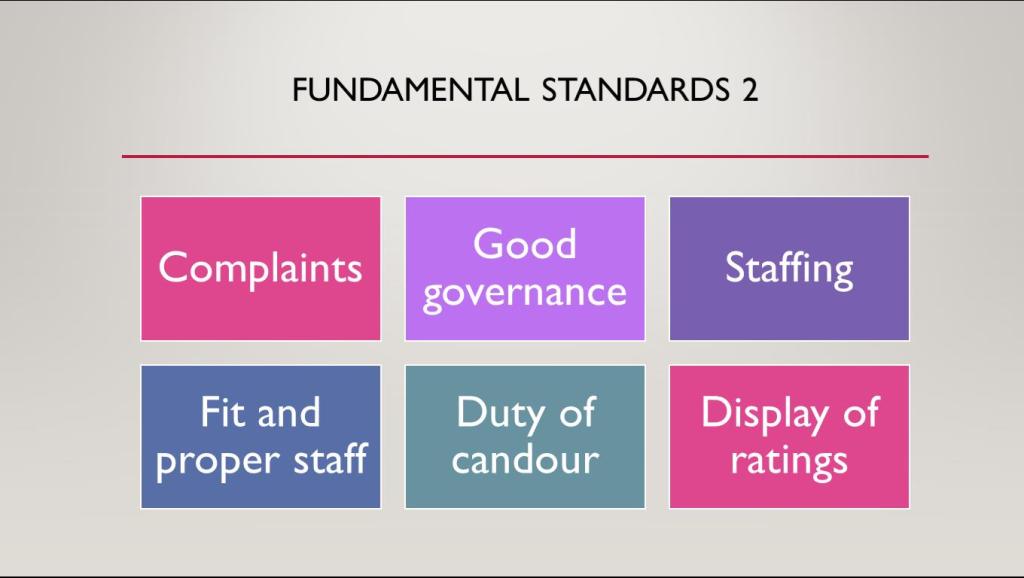
In cases of unresolved issues, escalating the complaint to regulatory bodies like the Health Service Ombudsman or Care Quality Commission (CQC) becomes necessary.

The Role of Regulatory Bodies
These bodies can investigate the case further, ensuring that the complaint is handled fairly. The CQC, although not handling individual complaints, can trigger inspections if there are significant failings in service provision.

When to Use Regulatory Bodies
This step is most appropriate for serious concerns such as poor care quality, negligence, or unsafe practices. Carers should be aware that investigations by these bodies can take considerable time.
Legal Action
Severe Level
When harm, serious malpractice, or gross negligence is involved, seeking legal advice may be the next appropriate step. This involves consulting a solicitor specializing in healthcare or mental health law.

Preparing for Legal Action
Selecting the right solicitor involves thorough research. Often, mental health law solicitors have extensive experience dealing with such cases and can offer valuable advice on the viability of pursuing legal action
When to Consider Legal Action
Legal action is usually reserved for extreme cases involving significant harm or death of the service user due to negligence or severe violations of rights. Legal channels can offer compensation and bring justice, albeit at a financial and emotional cost.
Public Campaigns and Media Attention
Escalation to Media and Public Campaigns
As a last resort, if internal and formal channels fail, bringing the issue to the public through media or social campaigns might be necessary. This becomes relevant when the issue represents a systematic failure affecting multiple service users or carers.

Steps to Engage Media or Public Campaigns
Carers can contact press organizations, social media channels, mental health advocates, or relevant charities, such as Mind or Rethink Mental Illness, to amplify their concerns.
The Role of MPs and Other Influential Bodies
Sometimes reaching out to local Members of Parliament (MPs) can also lend significant weight to a complaint, ensuring that it gets the attention it deserves. MPs can raise systemic issues within parliamentary forums, adding another layer of accountability for the service providers.

Summary
Navigating the complaint process within healthcare systems is a multi-tiered approach, designed to ensure that carers’ voices are heard at different levels of severity. Starting from informal resolutions, progressing to written complaints, and escalating to regulatory bodies or legal action, the system provides various stages for addressing concerns. If all else fails, public campaigns and media attention can serve as powerful tools to bring systemic issues to the forefront. Understanding these steps empowers carers to advocate effectively for their loved ones, ensuring that they receive the care and support they rightfully deserve.

By following this structured approach, unpaid carers can raise concerns at appropriate levels, ultimately ensuring that their voices are heard and acted upon, bringing about meaningful change in the system.
Remember complaining about a service is never that easy, full of stress and worries, but if we do not complain then how can health and social care services improve?
It is your right to complain as a carer if you are unhappy with results. Use it!!