
By Triangle of Care community chair Matthew McKenzie FRSA BEM
For the month of March, unpaid carers, NHS professionals, and key stakeholders came together for another Triangle of Care National Community Meeting, which is a powerful space of collaboration, reflection, and shared purpose. Chaired by Matthew, the meeting spotlighted significant developments in carer engagement, mental health service standards, and equity frameworks across the NHS.
From policy updates to practical implementation, the conversation echoed one key message: carers are essential, and their voices must be heard as part of the triangle
Expanding the Triangle: Updates from the Carers Trust
The meeting opened with comprehensive updates on Triangle of Care activities, delivered by Mary Patel from the Carers Trust. She highlighted progress made from January to March and outlined a bold agenda for the months ahead. Notably, 89% of NHS mental health trusts are now engaged with the Triangle of Care framework, which is a promising milestone.
A major focus this year is integrating the Patient and Carer Race Equality Framework (PCREF), which is set to become mandatory for all mental health trusts in England. Mary announced a collaborative pilot with 10 trusts, ensuring that race equality and carer inclusion go hand-in-hand.
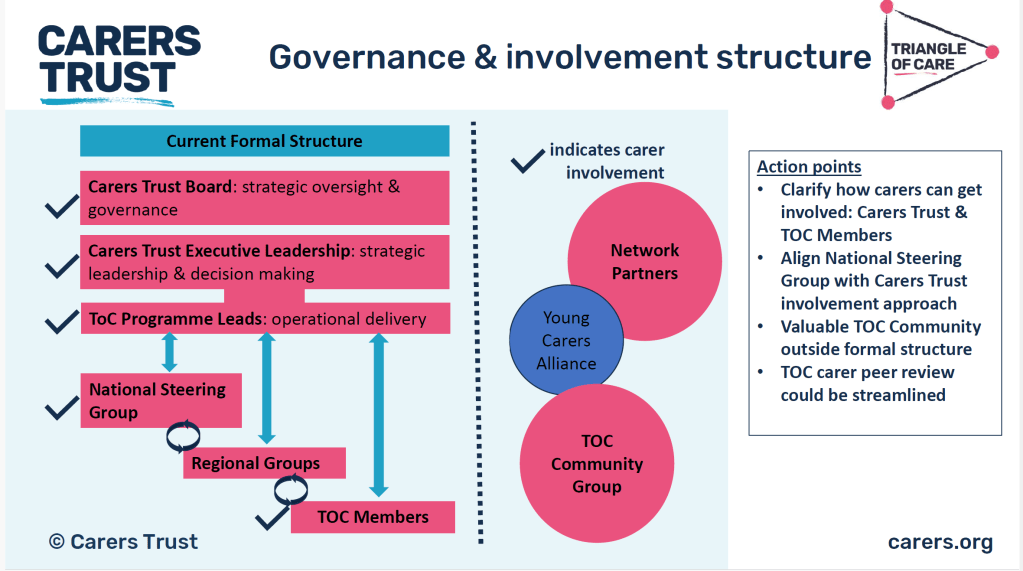
Plans are underway to embed the Triangle of Care group into formal governance structures, offering carers a tailored “menu” of involvement options and a peer-learning platform to enhance shared experiences and learning.
Mary also mentioned the need for training staff to treat carers equally, not just based on their skin color but also considering their cultural background. She emphasized that the pilot work is a slow process and aims to have draft guidance by the end of the year.
Incorporating PCREF
Anastasia, who is leading the work from a provider perspective, was invited to provide further information.
Anastasia from Avon & Whiltshire NHS Trust, speaking from a provider perspective, emphasized co-production and clear communication as non-negotiables for success. A carer raised an important point on language accessibility, and the use of translation tools like Recite Me was shared as a practical solution. Meanwhile, another carer highlighted a gap in supporting carers who are also patients, a topic taken up for further exploration.
Alan Worthington founder of Triangle of Care proposed a closer look at how general hospitals can better identify and support carers — starting with simple, achievable steps. Drawing on experience from Torquay, he emphasized that even small actions like providing information and recognition to carers can make a significant difference.
Matthew with Wendy Doyle who is the Public & Patient lead at St. George’s Univeristy hospital shared insight into their journey developing a Carer’s Charter in a hospital setting, emphasizing the role of hospitals in improving carer experience and visibility.

Building Skills, Shaping Futures: Nurse Training and Family Support

Catherine Gamble representing the Royal College of Nursing, provided a passionate overview of mental health nurse training programs and her ongoing work to support carers through professional development.
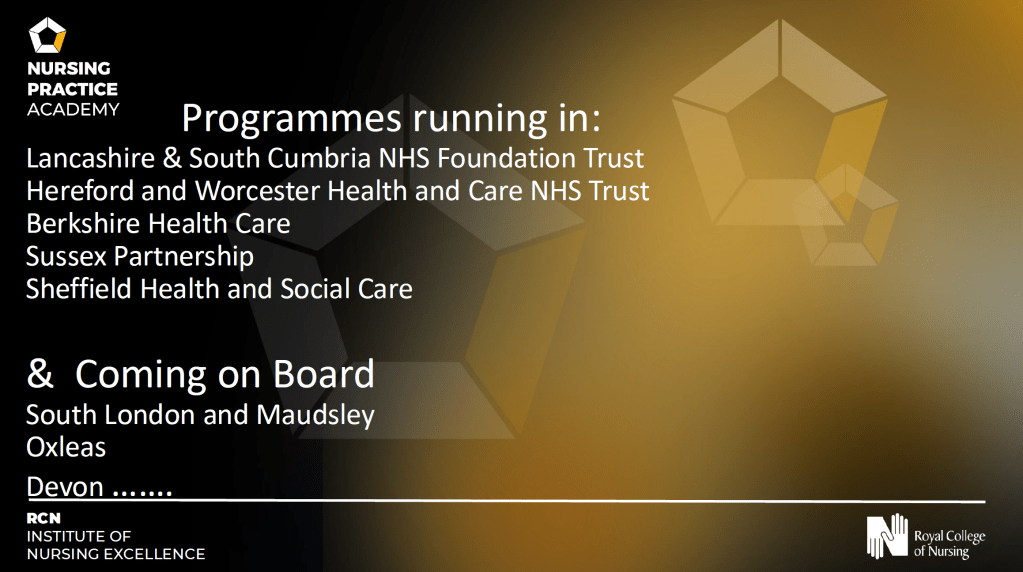
Catherine discussed her work with the Royal College of Nursing, focusing on the need for psychosocial interventions and training for mental health nurses. She mentioned a program rolling out across the country, with Matthew as a member of the steering committee. Catherine also addressed a carer’s question about promoting awareness to the community, mentioning various channels they use to raise awareness.
She introduced an Enhanced Family Support Program, offering informal practice, coaching, and role-play to build confidence in working with families.
With early positive feedback, the team is exploring recognition badges for trained nurses — echoing established models like the Admiral Nurse. A “butterfly image badge” is in development, celebrating commitment to carer inclusion and family support.
Catherine also shared progress on a continuing professional development curriculum, which is currently being adopted by several NHS trusts. Focused on supporting families and carers in the recovery journey, the curriculum helps nurses translate theory into compassionate, informed practice.
Challenging Inequality, Championing Consistency
Throughout the meeting, the group focused on issues like inconsistent service standards, the two-tier experience between trusts and commissioned services, and barriers faced by carers who are excluded from their loved ones’ care. The consensus? These challenges must be tackled through stronger partnerships, better training, and shared accountability.
Catherine also brought attention to dementia care, underlining the need for respectful, tailored communication with older adults. A new training course is on the horizon, aimed at equipping staff with the tools to better connect with and support this often-overlooked group.
Looking Ahead
The meeting closed on a hopeful note, with Matthew inviting participants to share resources and stay connected. There was energy around collaboration from future webinars to shared platforms and national recognition for carer-inclusive practices.
The Triangle of Care continues to grow in depth and reach, driven by a passionate community committed to improving outcomes for carers, patients, and professionals alike.
Together, we are building a mental health care system where no carer is left out and every voice is heard.