Welcome to a brief update of my ethnic mental health carers forum. For this month we were joined by South West London & St George research team. The team from a training company introduced a cultural capability training program aimed at reducing race and ethnic disparities in mental health care, while Matthew presented a summary of various reports highlighting health inequalities faced by ethnic minorities in the UK. The Forum also discussed the importance of advocacy for carers, the challenges of engaging with diverse communities. A carer from South Yorkshire also discussed the potential for setting up a group to support black people in the area.
Cultural Competence Training for Trusts
The training company introduced a cultural capability training program they are developing for the South West London and St. George’s Mental Health Trust. The program is part of an ethnicity and mental health improvement project and aims to reduce race and ethnic disparities in mental health care. Representatives from the team also discussed their evidence review on cultural competence in mental health care and their use of a model of cultural competence. The training is expected to impact staff, carers, and patients by promoting culturally sensitive care plans and reducing inequalities. The team also discussed the potential to tailor the training for other trusts.
Addressing Health Inequalities and Disparities
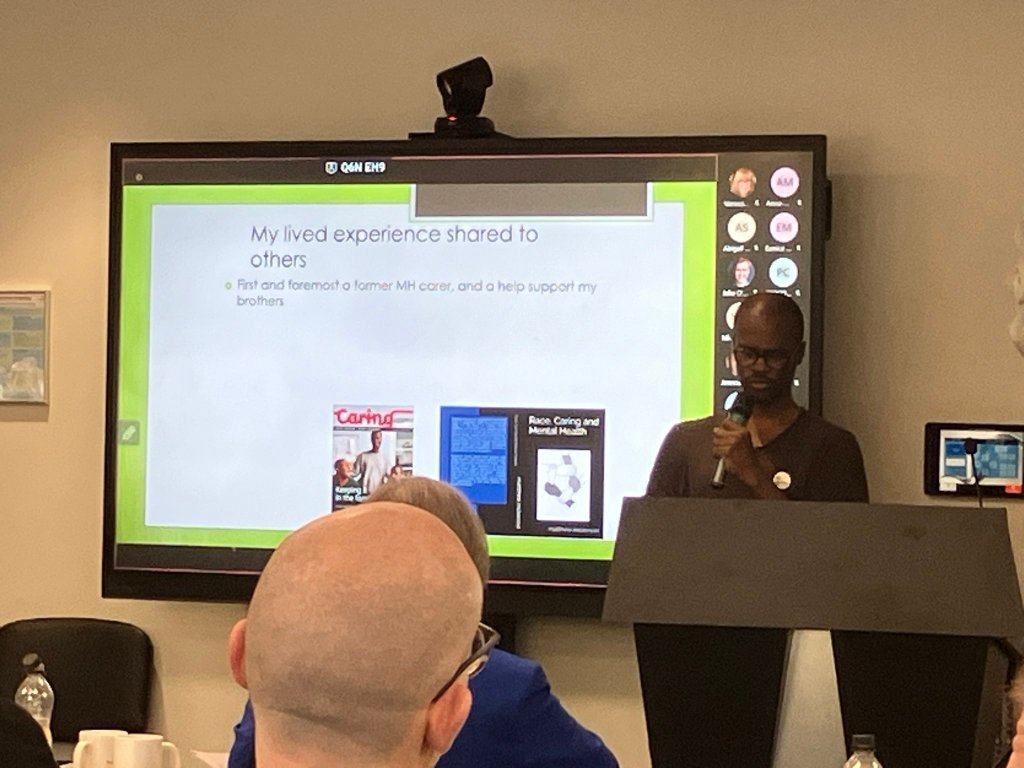
Matthew presented a summary of various reports highlighting health inequalities and disparities faced by ethnic minorities in the UK. He emphasized the importance of these reports in supporting the Patient Care Race Equality Framework (PCRF) and other initiatives addressing health inequalities, discrimination, and racism. The reports, from organizations such as the NHS Race and Health Observatory, Public Health England, and the CQC, demonstrate that ethnic minorities face higher risks with certain health conditions, barriers to accessing services, and poorer health outcomes.
Matthew also mentioned the role of institutional racism, socioeconomic disparities, and cultural barriers in perpetuating these disparities. He concluded by emphasizing the need for systematic reforms to ensure equitable health outcomes for all.
Addressing Healthcare Disparities and Trauma
Laura from Cygnet HealthCare expressed her appreciation for Matthew’s ability to present information in an understandable and accessible manner, which she believes is not done enough. She also highlighted the importance of Matthew’s role in educating others and ensuring the right actions are taken. A carer member of the group then brought up a report from the Race Equality Foundation and Learning Disability England, which highlighted disparities in access to healthcare for ethnic minorities with learning disabilities. She shared her personal experience of a young person with a learning disability, autism, and mental health issues facing challenges during the COVID-19 pandemic. The group acknowledged the system-generated trauma faced by carers and the need for more awareness and action on these issues.
Mental Health and Learning Disability Event
In the meeting, A carer highlighted the upcoming mental health and learning disability listening event, which was previously cancelled due to lack of awareness. Others at the meeting expressed their support for the event and the importance of advocating for carers.
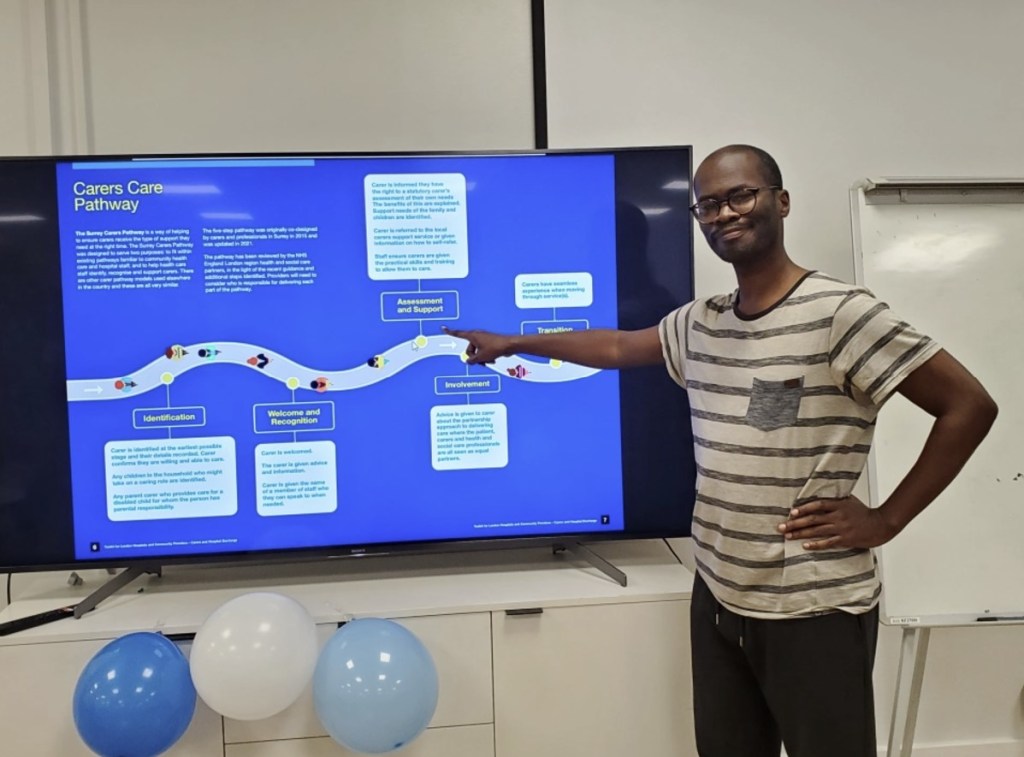
A representative from Surrey & Borders NHS trust who is the programme lead for carers and co-production, discussed the Trust’s co-production framework and their efforts to reach a diverse community for co-production opportunities. She also mentioned the Trust’s strategy to mirror the triangle of care. Matthew shared his experience at the Trust’s learning event and his plans to help promote the Trust’s work, particularly in relation to carer involvement.
Mental Health Event Postponement Concerns
A carer expressed surprise at the postponement of a mental health and learning disabilities listening event, which was initially scheduled for September. Another carer, who is relatively new to the Maudsley, had not been aware of the event’s postponement and was concerned about its lack of awareness. She had reached out to various individuals within the organization, including others, to discuss the event. Carers suggested that the carer should also speak to Zoe Reed or Shania, who are in charge of PCREF, to ensure the event’s success. The carer agreed to continue her efforts to promote the event and ensure its awareness.
Supporting Black Mental Health Groups
Carers discussed the potential for setting up a group to support black people in South Yorkshire, with Matthew suggesting that funding could be sought from the ICB and the charity associated with their NHS trust. A carer shared his experiences with a similar group in Peterborough, emphasizing the need for more conversation and less medication in mental health care for black people. A Carer, who is involved in setting up a group in Kent, shared her challenges due to the predominantly population in her area. Matthew also mentioned an upcoming event on the new Mental Health Act and its potential impact on carers. The team agreed to reconvene in January.