Chaired by Matthew McKenzie, Lived-Experience Carer
The latest meeting of the National Ethnic Mental Health Carer Forum brought together unpaid minority carers, community partners and four NHS mental Trusts (Avon & Whiltshire were kind enough to be included to update) to explore progress toward the Patient & Carer Race Equality Framework (PCREF), share challenges, and elevate lived-experience voices. As always, I ensured the space remained honest, fast-paced and rooted in what truly matters to ethnic minority carers: being heard, understood and included.
My latest blog for the November forum captures key highlights from each Trust, along with questions raised by attendees, reflecting the critical concerns and lived realities that continue to shape PCREF work across the country.
1. Avon & Wiltshire Mental Health Partnership Trust (AWP)
Focus: Triangle of Care, PCREF oversight, carer champion roles.
Avon & Wiltshire outlined how their PCREF programme is being driven through a clear governance structure, including a central Oversight Group and locality-based meetings. These layers ensure that learning from communities and staff filters upward and influences whole-trust priorities. Their collaboration with Nilaari (I think that is what their called), a long-standing community organisation supporting racially marginalised groups, has been key in grounding their PCREF work in authentic community voice.
A central pillar of their presentation was the strengthening of the Triangle of Care and carer-related PCREF oversight. They recognised that carer involvement cannot rely on goodwill or isolated champions; it requires structurally defined roles, written responsibilities, and consistent organisational expectations. The Trust is working on ensuring that every team and ward embeds a carer champion, whose purpose is not to “do everything for carers”, but to support cultural change within the workforce so that carers are recognised as equal partners.
They emphasised the importance of building staff capacity in cultural humility and safe conversations about race. AWP acknowledged that staff often feel unprepared to discuss ethnicity, discrimination or identity with carers. To address this, the Trust has created psychologically safe internal spaces, particularly for racially marginalised staff—to process experiences and explore how structural and interpersonal inequalities impact both staff wellbeing and patient care. This cultural environment is foundational to PCREF implementation because it shapes how confidently staff engage with diverse carers.
Key Points:
- Carer champions must support, not replace, teams in working with carers.
- Emphasis on psychological safety for racially marginalised staff and carers.
- Encouraging honest conversations around race, trauma, and culture across staff teams.
Questions raised by attendees:
- How do you embed cultural awareness within staff teams, not just for carers?
– Concern that staff dynamics and cultural differences must be addressed to create consistent culturally responsive care. - How do staff and leaders hold ‘difficult conversations’ about race and safety?
– Attendees wanted clarity on how psychological safety is practiced and how managers are supported.
🌟 2. Birmingham & Solihull Mental Health NHS FT
(Children & Young People’s Division – “Co-STARS” programme)
Birmingham & Solihull (CYP) presented one of the most detailed and emotionally grounded PCREF programmes, shaped heavily by lived-experience research with Black diaspora families. Their PCREF priorities, knowing our communities, transforming with communities, and delivering care that works reflect a commitment to embedding cultural responsiveness at every step. Their partnership with the University of Birmingham and Forward Thinking Birmingham has produced the Co-STARS project, a blend of lived-experience-led community work and staff training modules.

A major part of their PCREF advancement comes from working intensively with families to capture how racialised parents feel when using services. The Trust shared powerful testimonies from Black carers who described needing to “emotionally self-regulate” in meetings to avoid being labelled angry, unstable or cold. Parents also highlighted the emotional labour of protecting their children from stereotypes such as the “angry Black boy”, as well as fears of being adultified or dismissed. These insights have directly reshaped responses from clinical teams and informed the development of carers’ passports and safe spaces.
Birmingham & Solihull also emphasised building structures to ensure that their care pathways become culturally competent and adaptive. They are embedding PCREF champions across all clinical pathways, from eating disorders to psychosis and autism, ensuring diversity and inclusion principles shape every aspect of assessment, treatment and review. The Trust is also developing e-learning on culturally responsive practice, and expanding identity-specific support spaces (e.g., Black Carers Groups and new plans for Asian carers’ spaces). This multi-layered approach reflects a commitment to PCREF that is both structural and deeply relational.
Key Points:
- Embedding culturally competent conversations within CYP teams.
- Developing a Black Carers Group and safe spaces for racialised parent groups.
- New e-learning on culturally responsive practice (from Co-STARS package).
- Use of carer passports to ensure carers feel like equal partners.
- Strong focus on how ethnic minority parents feel judged or misread by services (e.g., “angry Black woman,” “cold mother”) – themes drawn directly from carer focus groups.
- Recognising adultification, stereotyping, and the emotional labour families perform.
Questions raised by attendees:
- What about older adult Black communities?
– Carers questioned how older Black adults, shaped by decades of racism, would be included in PCREF work. - Are you working with the police on cultural awareness?
– Concerns around disproportionate use of Section 136 and stereotypes (e.g., assuming someone is “aggressive” because they speak loudly or gesture). - How will parent–carer voices shape service pathways and outcomes across all diagnoses (e.g., autism, psychosis)?
3. Sussex Partnership NHS Foundation Trust
Sussex Partnership presented PCREF as a three-pillared programme: data, co-production & engagement, and workforce development. Their first priority is improving ethnicity and protected characteristics data, which they acknowledged has historically been inconsistent. Sussex is launching a behavioural-change campaign that involves interviewing service users from minority backgrounds about why they may decline to share ethnicity, alongside staff interviews to understand documentation issues. Their goal is a transparent baseline from which meaningful PCREF action can be driven.
The Trust also described significant investment in a new data infrastructure via Power BI dashboards. These tools will pull together real-time information on areas such as restraint, Section 132 rights, and involuntary detention by ethnicity. The Trust stressed that PCREF cannot function without high-quality data because inequalities must be clearly visible and accessible to teams at every level—from ward managers to executive boards. Their future ambition is to enable quicker identification of disparities and faster interventions that prevent harm.
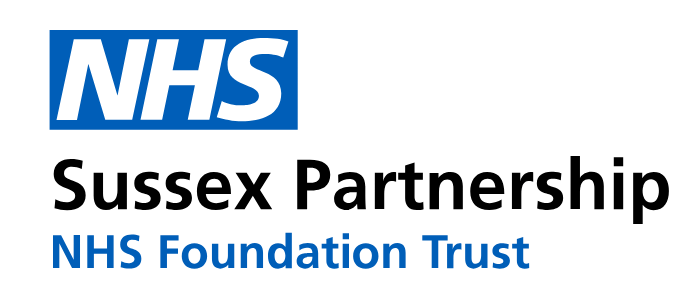
Sussex’s strongest focus was on building genuine co-production through their Expert Delivery Group (EDG). Unlike past approaches where community partners were only consulted, the EDG is designed as a collaborative decision-making space. Sussex acknowledged up front that phase 1 of PCREF planning did not fully embody equal partnership, and committed to ensuring that phase 2 will be co-produced from the ground up. The EDG will define what co-production means, co-design PCREF implementation plans, and shape updates that reflect community priorities, trust recovery, and anti-racist aspirations.
Key Points:
- A behavioural-change campaign to improve ethnicity data recording (currently 65% compliance).
- Development of Power BI dashboards for rapid inequality analysis.
- Defining anti-racist and cultural competency skills for staff, tied to new EDI training.
- Creation of the Expert Delivery Group (EDG) as a collaborative community–trust space.
Questions raised by attendees:
- Is this “real” co-production or consultation?
– Attendees challenged Sussex on whether the initial plan was created with the community or presented to them. - How will service users and carers hold equal power within co-production?
- How will your anti-racism ambitions be demonstrated externally to communities?
– Attendees expressed concerns that staff training alone does not reassure communities. - How will carers’ needs be embedded in PCREF (Triangle of Care)?
🌟 4. Kent & Medway Mental Health NHS Trust
Presenter: Kamellia (with contribution from Harriet – Lived Experience)

Kent & Medway showcased a comprehensive and governance-driven PCREF structure supported by their Equity for All Assurance Group. The Trust has embedded health inequalities into its broader strategy and is working to ensure that PCREF, protected characteristics data and health equity are woven into everyday practice. With the Trust’s newly updated name and identity, PCREF sits at the centre of a renewed commitment to equitable access, outcomes and patient experience across Kent and Medway.
Their PCREF progress includes delivering cultural competence training to 259 senior leaders, a significant investment in shifting leadership behaviour and expectations. They have also identified major data disparities in areas such as complaints, where ethnicity recording is only around 30%. To address this, they are rolling out the About Me form across their clinical system (Rio), which streamlines demographic and protected characteristics documentation for both carers and patients. This step is being supported by staff training designed to build confidence in discussing sensitive identity-related topics.
Kent & Medway also highlighted the expansion of their new Involvement & Engagement Team, which links directly with communities across East, West and North Kent. They are testing a Health Inequalities Toolkit, improving carer experience data collection, and creating new Family, Friends & Carers forms that capture protected characteristics, communication needs, and whether a carers pack was offered. The Trust’s approach is detailed, structural and long-term, aiming to embed PCREF as part of “business as usual” rather than a separate initiative.
Key Points:
- 259 senior leaders trained in cultural competence.
- New About Me demographic/protected characteristics form launching trust-wide.
- Major data gaps identified (e.g., only 30% ethnicity data for complaints).
- New Involvement & Engagement Team connecting with community groups.
- Testing the Health Inequalities Toolkit .
- New Family, Friends & Carers Information Form including carer-pack tracking.
Questions raised by attendees:
- Do you provide information in languages other than English?
– Carers stressed that if translations don’t exist, PCREF is inaccessible from the start. - How will carers be supported to attend meetings given their unpredictable caring responsibilities?
- How will you gather demographic data for carers when many do not have Rio records?
- How will minority groups be reached in areas where the Trust’s population is overwhelmingly White British?
5. Carer Support Organisation (Kent & Medway Carers Support)
Presenter: Donna Green (involve Kent)

Key Points:
- They run trust-wide carer experience groups and targeted workshops.
- Emphasised difficulty for carers to attend meetings due to constant demands.
- Highlighted the need for multiple approaches, including creative well-being sessions.
Closing Reflections from the Forum
I wrapped up the session acknowledging:
- The strong desire across Trusts to improve PCREF delivery.
- The pressure to progress quickly without losing sight of lived experience leadership.
- The need to bring CQC into future meetings for transparency around expectations.
- The importance of ethnic minority carers having a forum that values honesty over polished presentations.
Final Thoughts
This month’s forum demonstrated that while progress continues nationally, there remain shared challenges across NHS Mental HealthTrusts:
- Recording ethnicity and protected characteristics meaningfully
- Embedding anti-racism beyond training modules
- Meeting the needs of Black, Asian and other racialised carers
- Co-production that is real, not rhetorical
- Involving carers whose time and emotional capacity are already stretched
- Ensuring safety, trust and humanity in every interaction.
Above all, the session showed that ethnic minority carers are not passive observers they’re leading, questioning, shaping and insisting on accountability at every step.