Posted: July 2025
By: Matthew McKenzie
In July 2025, we held another meeting of the London Hospital Discharge Carers Forum, which brings together carer centres, NHS professionals, and lived experienced unpaid carers to explore how we can better support unpaid carers through the complex hospital discharge journey.
With key developments shared, questions raised, and future opportunities on the table, I’m sharing this blog to ensure everyone is informed.
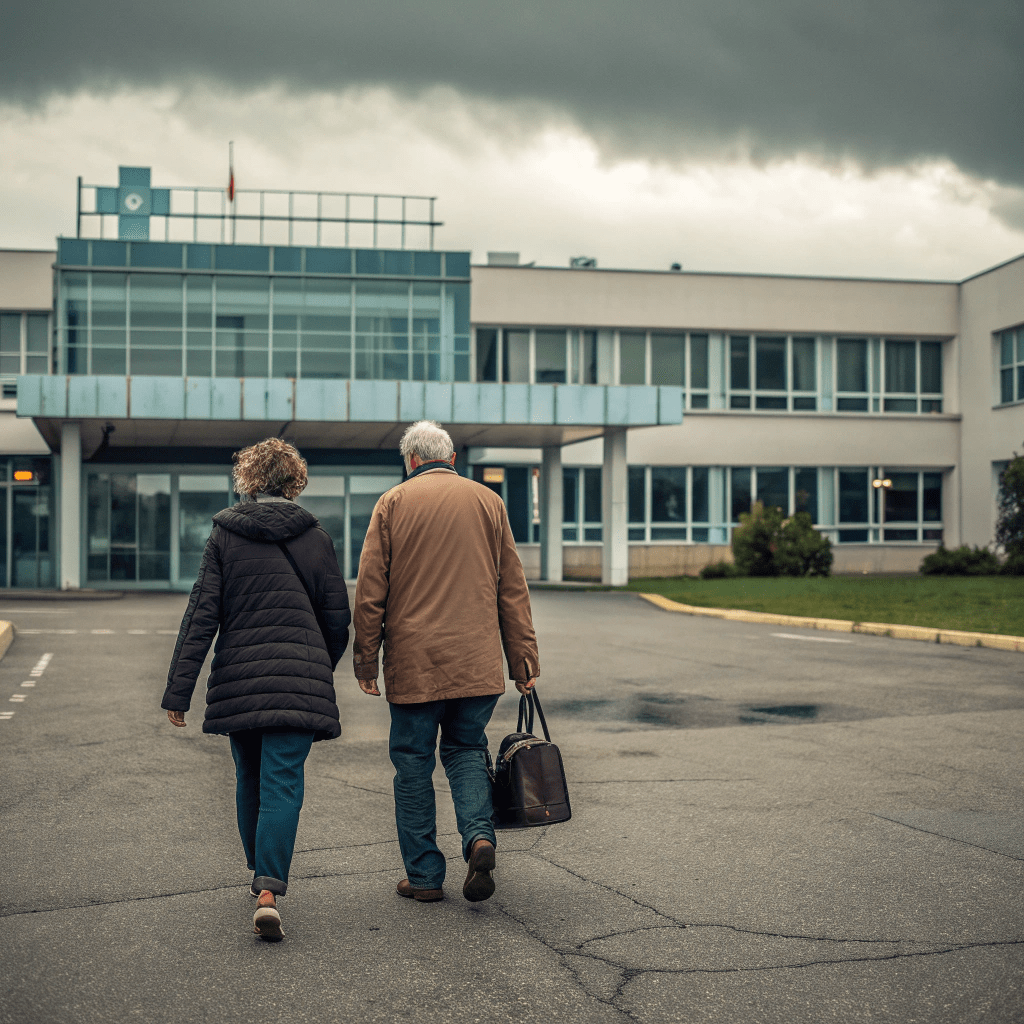
A Focus on Hospital Discharge but With Carers at the Centre
The forum continues to highlight how vital carer centres are in delivering effective, compassionate discharge support. But alongside that recognition comes rising expectations: better digital access, stronger links with acute hospital teams, more formal involvement in care planning, and even new digital tools to manage carer identity and input.
Our role is growing and so is the need for collective visibility and coordinated action.
Key Themes from July’s Discussion
1. NHS England Hospital Discharge Toolkit & Care Contingency Plan
As an involved carer, I delivered the NHS England update. The main message? The Care Contingency Plan (CCP) is becoming a key focus across the system. There are planning sessions due in September, and carer centres might be asked whether they can take on CCP delivery alongside existing carers assessments.
This triggered a crucial question: Will additional funding or contractual support be offered to carer centres taking on CCPs? because we can’t afford to quietly absorb additional workload without clarity on resources or expectations.
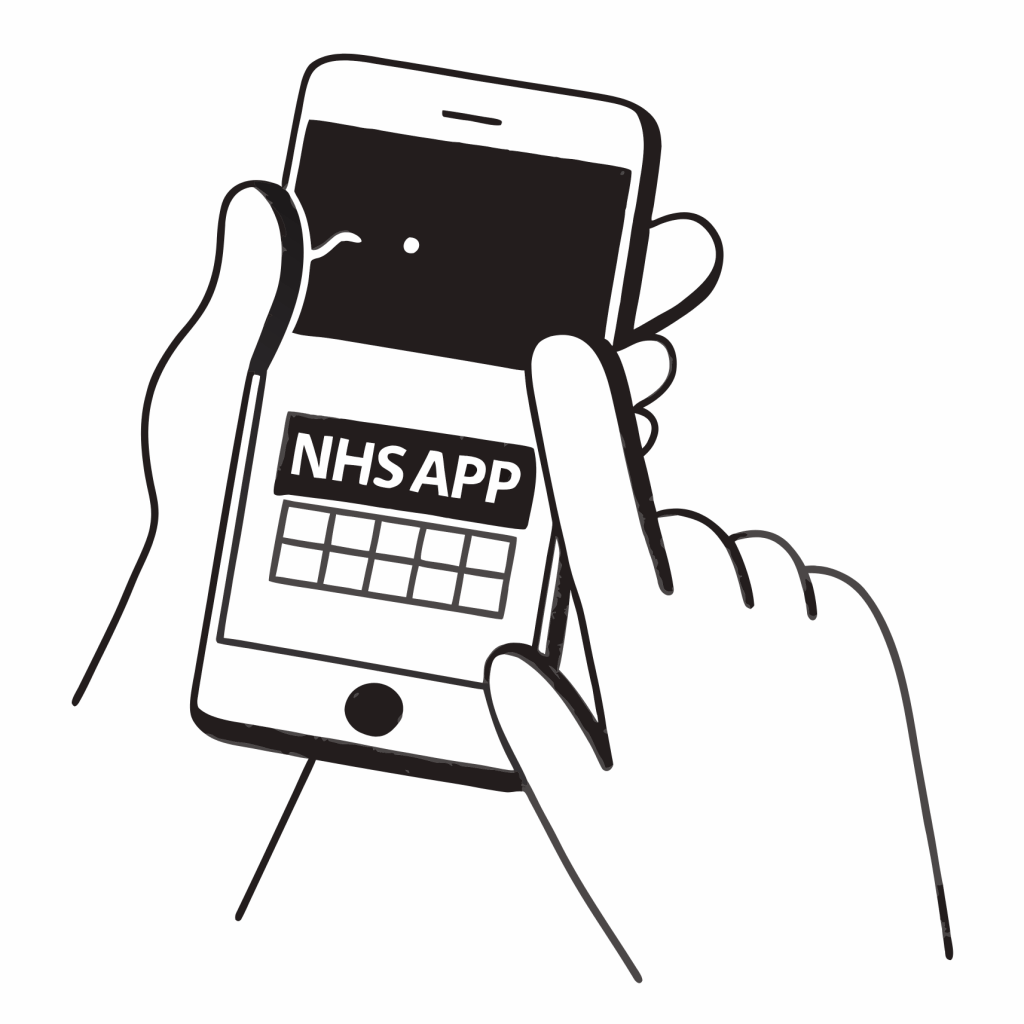
2. Digital Tools – NHS App & Carer Self-Identification
With the growing digitisation of NHS services, there are plans to enable carers to self-identify via a digital route. The Universal Care Plan (UCP) is being built into the NHS app, but there’s confusion about whether a separate “carer app” is being developed too.
We’ve asked NHS England for clarification: Will carers be expected to use one NHS app to manage both contingency plans and carer registration, or will multiple systems be introduced? The answer will have implications for how we support carers with digital skills and accessibility.
3. The Bigger Picture – NHS 10-Year Plan and Local Adaptation
We explored how the new 10-Year NHS Plan mentions carers primarily in the context of discharge, but offers little in terms of direct support or investment in carers themselves. Several carer centres raised concerns about being seen only as a means to improve discharge outcomes, rather than as partners in their own right.
That said, some centres are using the plan as an opportunity, working with local Integrated Care Boards (ICBs) to adapt and influence how the priorities are rolled out locally, including integration with neighbourhood health centres and walk-in clinics.
Peer Learning and Local Centre Updates
As always, our meeting included practical insights from carer centres embedded in local hospitals. Topics included:

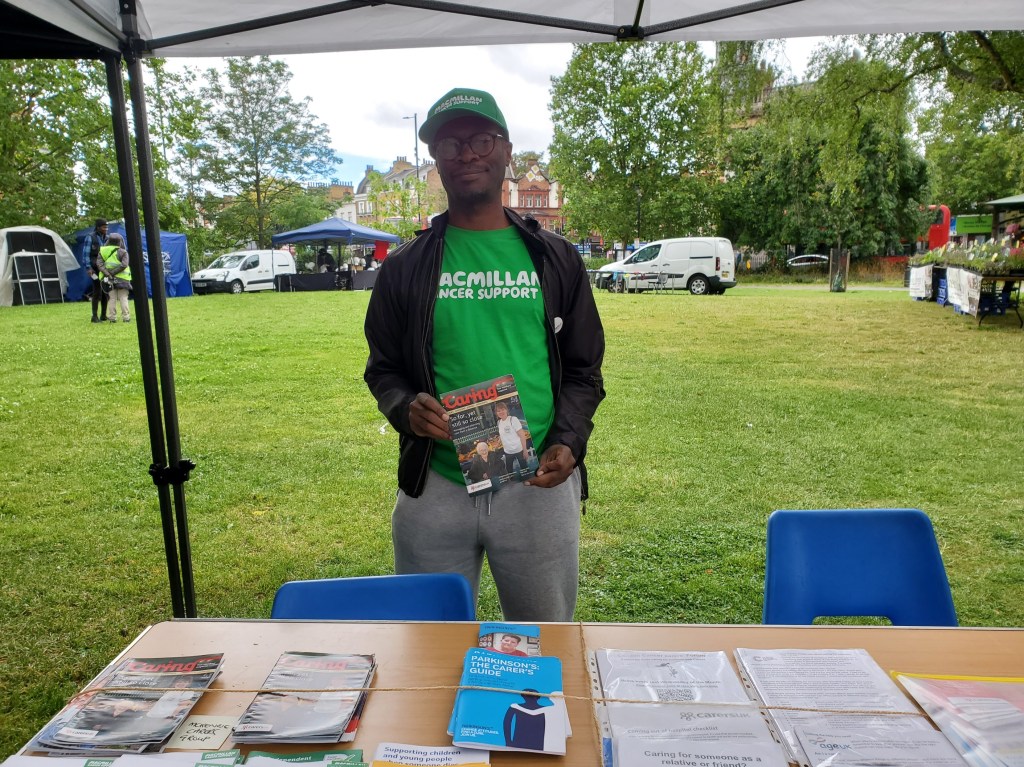
- Establishing hospital-based carer hubs and information desks.
- Hosting monthly drop-ins for carers on specific wards (e.g. stroke and frailty).
- Using ward rounds to identify and build relationships with staff willing to act as carer champions.
- Overcoming challenges in gaining visibility, sustaining presence, or maintaining resource levels for in-hospital work.
- Planning carers coffee mornings and pop-up stands to increase footfall and engagement.
For newer hospital-based carer workers, this space proved invaluable as a place to learn from colleagues, gather ideas, and avoid isolation.
Project Developments: What Centres Need to Know
Several borough-wide and London-wide initiatives are taking shape that could directly affect how carer centres operate in coming months:
- A standard operating procedure for hospital discharge, currently being developed across South East London, is aiming to streamline how carers are engaged at discharge, with pilot sites starting this September.
- In North Central London, work is underway on a web portal that makes it easier for hospital and emergency staff to refer carers into local support services including from the London Ambulance Service.
- Carer Centres in several areas are starting or refreshing carer charters, carer passports, and surveys designed to codify carer involvement and measure experience across hospital pathways.
- Carer support workers at one major South London hospital are re-establishing visibility post-staff transition. Efforts are underway to build new ward-level relationships and identify carer champions among staff. The centre is also exploring monthly carer drop-ins, asking the group for ideas on what works well and what doesn’t.
- One East London carer centre has established a hospital-based hub on a specific ward floor, acting as a go-to space for carers needing support or information. They also run monthly drop-in sessions on elderly/frailty and stroke wards conditions where family involvement in discharge planning is often critical.
These projects are at different stages, but all point to one thing: carer centres are being asked to operate more visibly, more formally, and more digitally. It’s essential we shape this process and not just respond to it.
With NHS England’s CCP work moving fast and carer integration into digital systems ramping up, carer centres can no longer afford to remain on the sidelines.
- We have a chance to be informed of policy changes early not after implementation.
- Carer centres and hospitals can raise concerns about workload, training, and funding before it’s too late.
- Newer or isolated workers benefit from collective knowledge-sharing and support.
This is not just another meeting, it’s one of the few cross-borough forums focused squarely on carer centres in the acute hospital context.
Looking Ahead: September Session
Our next meeting will be held usually the last week of September.
Let’s not let carers be an afterthought. Let’s make sure carer centres are seen, heard, and properly resourced.