Chair: Matthew McKenzie
Purpose of the Meeting
I chaired this meeting to bring together carers’ organisations, hospital representatives, commissioners, and system partners to share updates on how unpaid carers are being identified, supported, and involved in acute hospital settings. While hospital discharge was a central theme, I emphasised that meaningful carer involvement must begin at admission and continue throughout a person’s hospital journey and transition back into the community.
Attendance
- Matthew McKenzie – Chair
- Representative, Unpaid Carer / Healthwatch
- Representative, Greenwich Carers Centre
- Representative, Ealing Carers Partnership (includes Hillingdon)
- Representative, Lambeth Carers Hub
- Representative, Richmond Carers Centre
- Representative, Harrow Carers
- Representative, Camden Carers
- Representative, Imago Carers Services
- Representative, North Central London Carers Project
- Representative, Local Authority Commissioning
- Representative, Hospital Patient Experience Lead
(Apologies were received from additional ICB and system partners.)
Unpaid Carer / Healthwatch Representative
The unpaid carer representative shared lived experience insights highlighting that carers are still inconsistently identified across primary care and hospital settings. While there are pilots, policies and system intentions in place, carers frequently report feeling excluded from discussions about care and discharge planning.
They described how carers often struggle to obtain timely and accurate information, particularly during periods of crisis. Many carers are left unsure who to contact within hospitals, and communication is often fragmented or reactive rather than planned.
The representative also noted that progress frequently depends on individual staff champions rather than embedded systems. Without consistent hospital-based carer support, carers are left to advocate for themselves at times when they are already under significant emotional strain.
Lambeth Carers Hub
Lambeth Carers Hub provided a detailed update on their hospital-based carers support service operating across King’s College Hospital and Guy’s & St Thomas’. Their work focuses on identifying unpaid carers early, offering emotional and practical support, and ensuring carers are meaningfully involved in discharge planning and decision-making. Key activities include ward rounds, attendance at discharge and multidisciplinary meetings, safeguarding support, advocacy, and referrals into adult social care and community-based services.
They emphasised that having a consistent physical presence within hospitals has been critical to building trust with both carers and clinical staff. This approach has led to increased referrals, earlier engagement with carers, and improved communication between carers and hospital teams. The Hub also delivers carers awareness training to hospital staff, helping professionals better understand carers’ rights and roles, and creating internal champions within teams.
Despite strong outcomes, ICB working with Lambeth carers hub raised serious concerns about sustainability. Current funding for the hospital-based service is due to end in March, with no guarantee of continuation. They stressed that losing this service would represent a significant step backwards for carer involvement in hospitals, particularly given the clear evidence that early identification and support reduce carer stress and improve discharge outcomes.
Richmond Carers Centre
The Richmond Carers Centre representative explained that their service currently operates in a largely reactive capacity, with referrals typically received at or near the point of discharge. Support includes emotional support, carers’ rights workshops, dementia-focused information sessions, carers assessments and financial guidance.
They noted that carers often approach the service feeling overwhelmed following discharge, having had limited involvement in planning while their loved one was in hospital. This can increase pressure on carers once the person returns home.
The representative acknowledged that the absence of a regular hospital presence limits early engagement with carers. Opportunities were identified to strengthen strategic links with the Integrated Care Board and learn from boroughs where hospital-based models are already established.
Greenwich Carers Centre
The Greenwich Carers Centre representative reported that while carers often experience poor communication from hospital staff and feel excluded from discharge planning, the Centre plays a key role in supporting carers through these challenges. Many carers approach Greenwich Carers feeling anxious or overwhelmed after receiving late or unclear information about discharge, and the service works quickly to help them understand their rights and options.
As a small organisation without a permanent hospital presence, Greenwich Carers is frequently brought in once situations have already escalated. Despite this, the team provides strong advocacy and practical support, including contacting hospital staff on carers’ behalf, helping carers articulate concerns, and ensuring their voices are heard wherever possible.
The representative also highlighted the Centre’s commitment to empowering carers by supporting them to prepare questions, understand processes, and engage more confidently with professionals. While acknowledging that carers should not have to carry this burden alone, Greenwich Carers continues to offer reassurance, guidance and emotional support at some of the most stressful points in a carer’s journey.
Greenwich Council – Commissioning
The Greenwich commissioning representative provided a detailed update on current and planned work to review and re-commission carers support services, with contracts due to end in 2027. A central aim of this work is to gain a much clearer understanding of carers’ lived experiences across the whole system, including primary care, hospitals, discharge pathways and support once people return home. Hospital engagement and discharge were identified as critical pressure points for carers and a priority area for learning.
The representative emphasised that carers’ voices must shape future commissioning decisions, not just through surveys but via direct engagement with carers in existing groups, forums, workshops and one-to-one conversations. There was a clear call-out to partners to help identify opportunities to meet carers where they already are, including within community groups, peer support spaces and carers organisations. This engagement will help commissioners understand what is and is not working, and where carers experience the greatest barriers.
An update was also provided on work relating to the hospital discharge standard operating procedure developed across South East London. While Greenwich did not take part in earlier pilots, the commissioning team is now exploring how this resource can be implemented locally in a way that is meaningful and realistic within busy acute settings. This includes building on existing initiatives, such as carers charters and specialist nursing roles, and avoiding approaches that become tokenistic or are not properly embedded.
The representative acknowledged the challenges of engaging hospitals at pace, particularly given operational pressures, workforce constraints and wider system reform. However, they stressed that commissioning has a key role in creating the conditions for improvement by setting clear expectations, supporting partnership working, and ensuring carers are explicitly considered in pathways and service design rather than treated as an afterthought.
Harrow Carers
The Harrow Carers representative shared the impact of losing funding for a dedicated hospital carer support role. When the role existed, there had been strong engagement with discharge teams and improved staff awareness of carers’ rights and needs. Since the funding ended, there is no longer a consistent carer presence within the hospital. This has resulted in reduced engagement with carers and fewer opportunities to influence discharge planning.
The representative stressed that carers value continuity of support from hospital into the community. Without hospital-based roles, carers often experience a sudden and unsupported transition once their loved one is discharged.
Camden Carers
The Camden Carers representative confirmed there is currently no dedicated hospital engagement or discharge support service due to funding constraints. Previous hospital awareness work had to stop, limiting opportunities to identify carers early.
Camden Carers now focuses on community-based support, including carers assessments, information and advice, counselling, employment support and wellbeing services. These services remain well-used and valued by carers.
Attending the meeting was described as helpful for learning about hospital-based models in other boroughs. The representative expressed interest in exploring whether similar approaches could be developed in the future if funding allows.
Imago Carers Services
Imago provided a detailed update on their work supporting unpaid carers across multiple boroughs, with a strong focus on hospital navigation and safe discharge. They currently deliver carers services in Lewisham and the City of London, and are expanding work in other areas, including Havering. In the City of London, Imago works closely with adult social care and hospital discharge teams across several acute trusts, supporting carers whose loved ones are admitted outside their home borough.
A key strength of Imago’s model is their close operational relationship with hospital discharge teams, which allows carers to be identified earlier and supported more consistently through the transition from hospital to home. This includes practical guidance, emotional support, referrals for carers assessments, and rapid follow-up once someone is discharged. Imago highlighted that where they are embedded in discharge pathways, carers experience fewer delays, clearer communication and improved continuity of support into the community.
Imago also reflected on ongoing challenges, particularly that carers are still too often signposted rather than formally referred by hospitals. They are working with commissioners and hospital partners to address this by improving referral processes and developing clearer information for professionals. This includes new resources aimed at hospitals and GP surgeries, focused on carers’ rights, identification, and support within the health system. While progress is being made, Imago stressed that sustainable funding and system-wide commitment are essential to move beyond short-term pilots and ensure carers are consistently recognised as key partners in care.
North Central London Carers Project
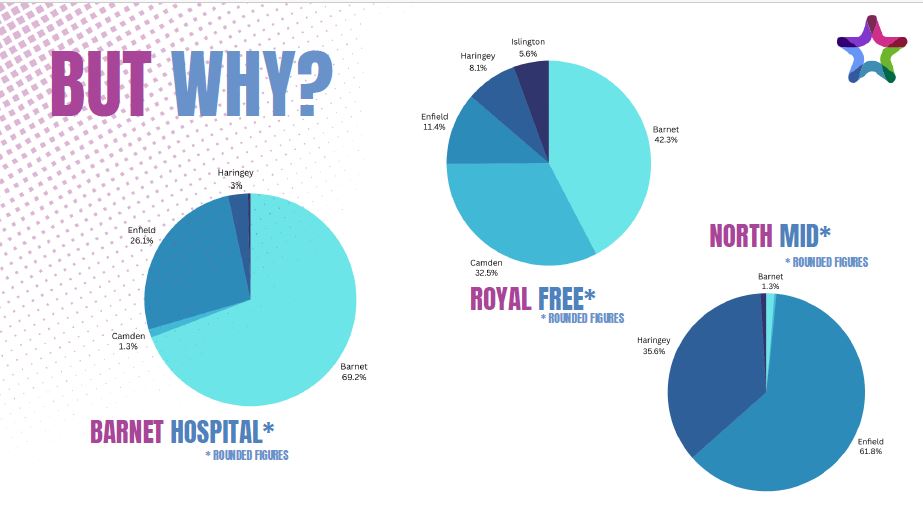
The North Central London Carers Project representative provided an update on work taking place across Barnet, Camden, Enfield, Haringey and Islington. The project focuses on improving referral pathways from hospitals and health services into local carers organisations, particularly where staff are unsure which carers service covers which borough.
They described the development of a single referral route designed to make it easier for hospital professionals to connect carers with the correct local support quickly and accurately. This work is intended to address one of the most common barriers carers face: delays and confusion caused by fragmented systems across borough boundaries.
The representative acknowledged that progress is being made in a very challenging environment, with significant pressures on NHS and local authority partners. However, there have been positive developments, including growing engagement from patient experience teams and plans to showcase collaborative work with NHS colleagues at London-wide events, demonstrating that sustained partnership working can lead to meaningful change for carers. This work involves close engagement with hospitals across North Central London, including the Royal Free London Trust (covering sites such as Royal Free Hospital, Whittington Hospital and Barnet Hospital), to strengthen referral pathways and improve carers’ access to local support.
Hospital Patient Experience Representative
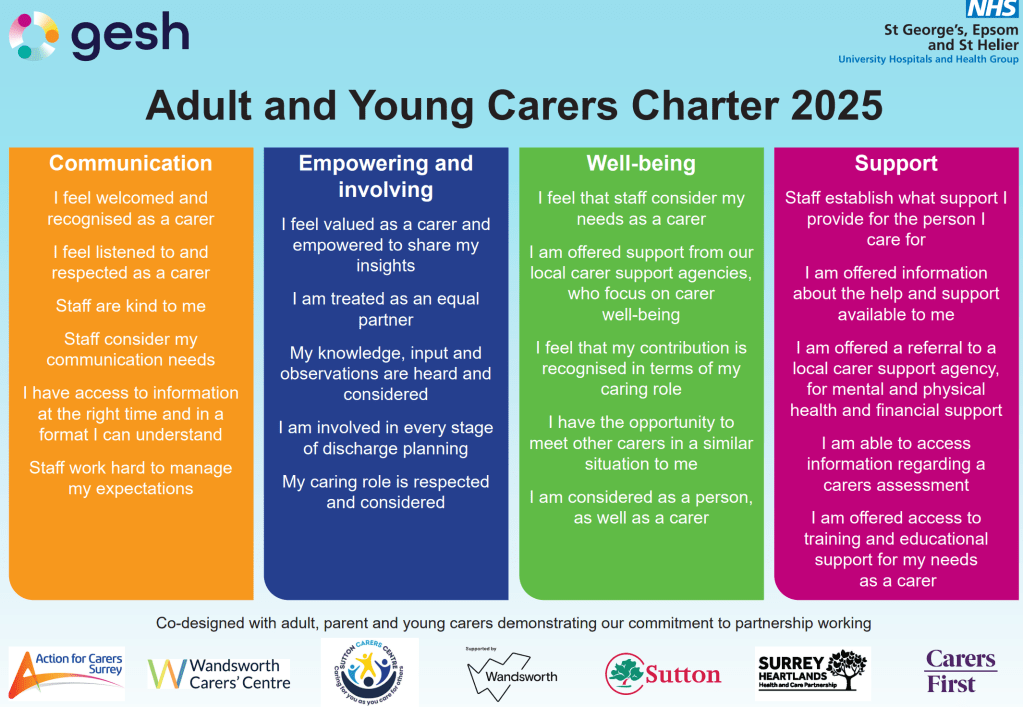
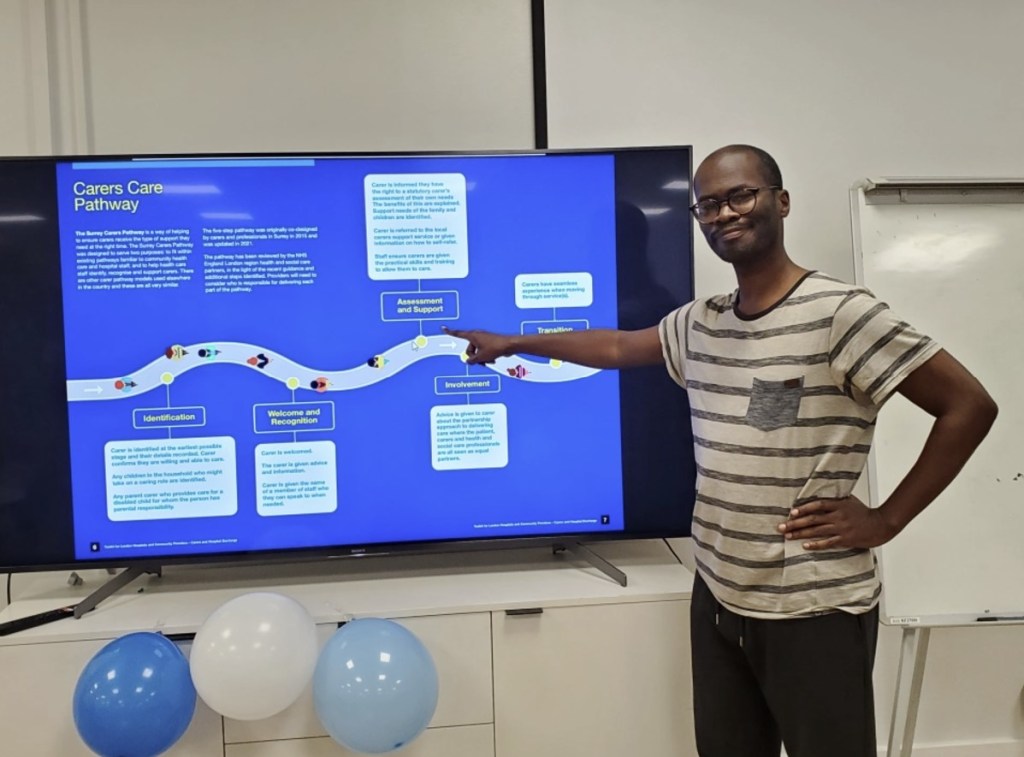
The hospital patient experience representative from George’s, Epsom and St Helier Hospitals (GESH) provided a detailed update on progress within their trust to improve identification and support for unpaid carers. This includes the co-production of a carers charter, developed directly with carers, setting out clear expectations for how carers should be recognised and supported.
They outlined the development of a carers policy and standard operating procedures, alongside staff training and e-learning. Carer identification and recording are being embedded into routine hospital audits, helping ensure carers are consistently recognised across services.
Further work includes carer surveys, dedicated carer forums, information boards, and plans to link carer identification to accreditation processes. This approach is intended to move carer involvement into business-as-usual practice and reduce reliance on individual champions alone.
Events and Shared Information
During the meeting, there was shared information about upcoming London-wide events focused on unpaid carers, particularly those aimed at influencing system change and strengthening collaboration between carers organisations and NHS partners. An upcoming Caring Across London event organised through Carers Trust was highlighted as an important opportunity to showcase good practice, hear directly from carers organisations and NHS colleagues, and raise issues around hospital engagement and discharge at a strategic level. Several attendees confirmed they would be attending or were interested in receiving further details.
It was also noted that colleagues from North Central London will be presenting jointly with NHS patient experience representatives at a London-wide carers event, demonstrating collaborative working between carers organisations and hospital trusts. This was shared as a positive example of how partnership approaches can influence wider system thinking and raise the profile of carers within acute settings.
In addition, links and information were shared relating to carers charters, standard operating procedures, hospital discharge toolkits, and evidence submitted to London-level discussions on unpaid carers. I encouraged attendees to review and share these resources within their own organisations and networks, as they provide practical examples that can be adapted locally. I also confirmed that I am happy to circulate any event details, articles or resources discussed so that those unable to attend meetings or events can remain informed and connected.
Useful Links and Further Information
🔹 London-wide Events and Policy Discussions
Caring Across London: Collaborating for Change (Carers Trust Conference)
https://carers.org/conferences/caring-across-london-collaborating-for-change
London Assembly Investigation – Experiences of Unpaid Carers in London
https://www.london.gov.uk/who-we-are/what-london-assembly-does/london-assembly-work/london-assembly-current-investigations/experiences-unpaid-carers-London
BBC News – Coverage of Unpaid Carers in London
https://www.bbc.co.uk/news/articles/c2e1n3rddzro
MyLondon – London’s Hidden Unpaid Carers
https://www.mylondon.news/news/zone-1-news/londons-hidden-unpaid-carers-living-33230856
🔹 Hospital Discharge, NHS and System Guidance
NHS England (London) – Carers and Hospital Discharge
https://www.england.nhs.uk/london/our-work/carers-and-hospital-discharge/
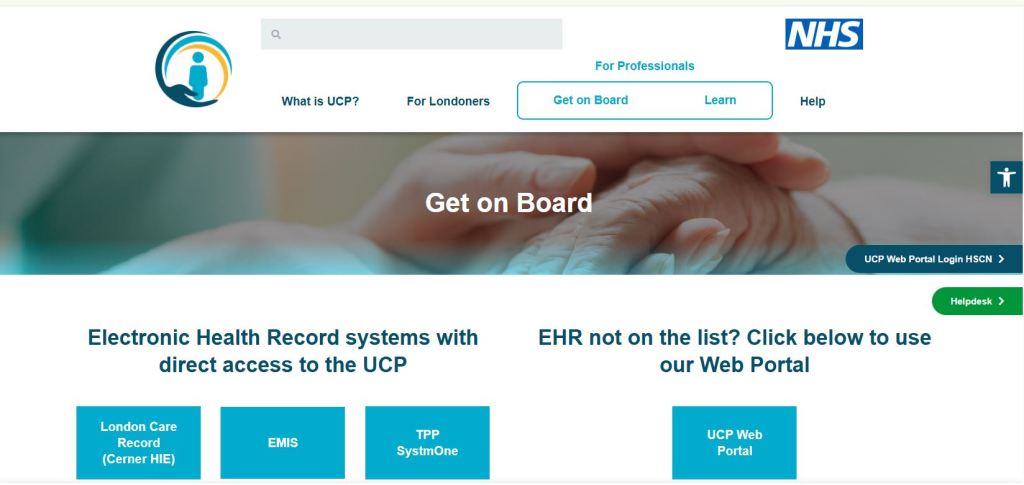
One London – Universal Care Plans (UCP)
https://ucp.onelondon.online/about/
🔹 Carers Rights, Frameworks and Good Practice
Triangle of Care (Carers Trust)
https://carers.org/triangle-of-care/the-triangle-of-care
Adult and Young Carers Charter (GESH – George’s, Epsom & St Helier Hospitals)
(Shared in the meeting by the hospital patient experience representative)
📄 Adult-and-Young-Carers-Charter-2025.pdf
🔹 Tools and Platforms Mentioned
Bridgit Care (used by Harrow Carers and others)
https://www.bridgit.care