By Matthew McKenzie – Triangle of Care Community Chair.
The meeting opened with a welcome to carers, professionals, and partner organisations, reinforcing the importance of the Community Group as a collaborative and inclusive space. The Chair highlighted the ongoing commitment to co-production, ensuring that lived experience remains central to all Triangle of Care development and decision-making.

The purpose of the meeting was outlined, with emphasis on shared learning, constructive challenge, and influencing national work. Members were reminded that discussions within the group directly inform improvements to Triangle of Care standards, guidance, and implementation across services.
2. Triangle of Care Update (with Q&A)
Mary Patel – Carers Trust
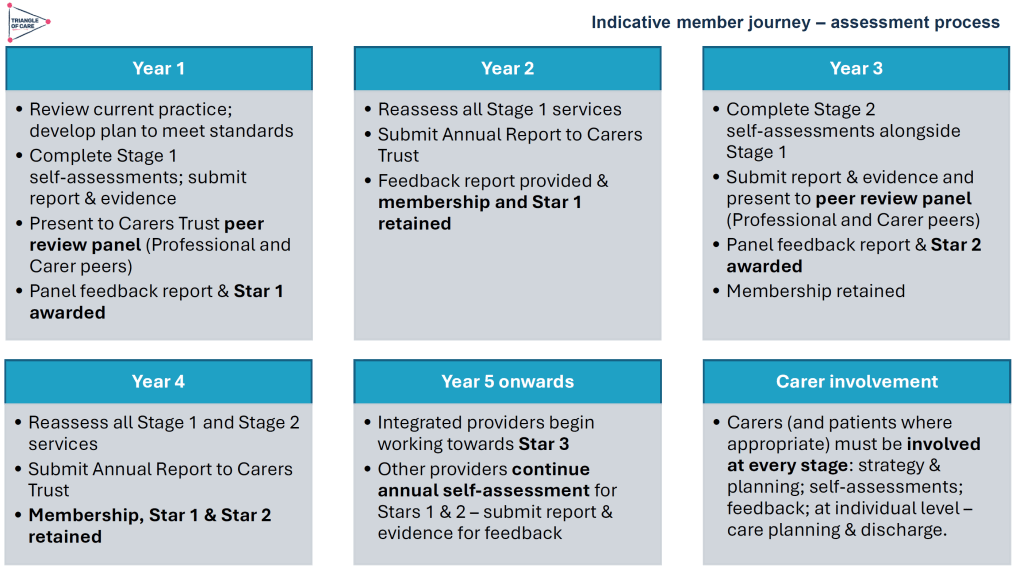
The Triangle of Care update focused on how the programme continues to evolve as a learning-led, improvement-focused framework rather than a compliance or inspection tool. Members were reminded that the Triangle of Care is designed to support services to reflect honestly on how well carers are recognised, involved, and supported, and to identify practical actions for improvement.
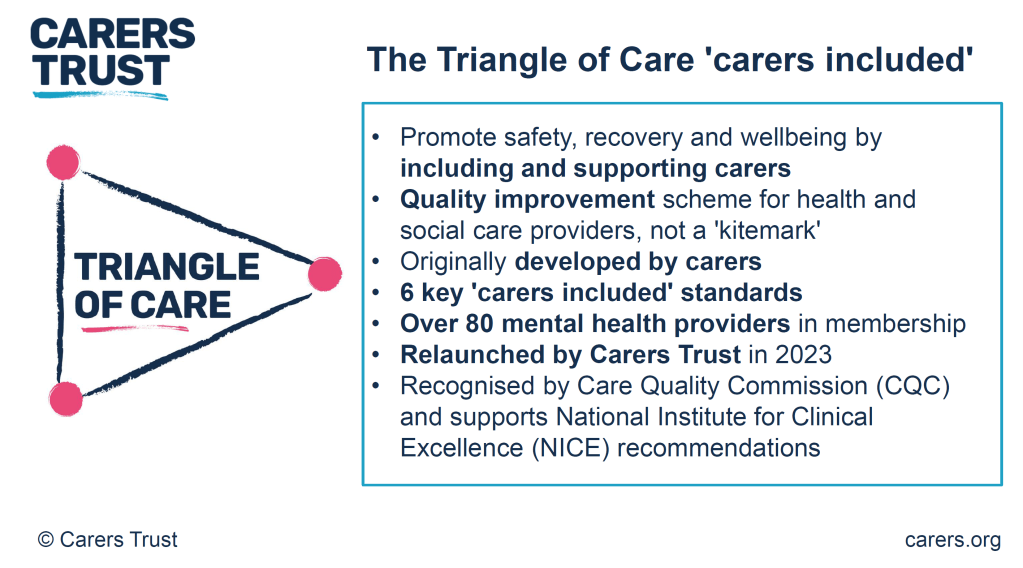
The update highlighted the growing maturity of the self-assessment and peer review process. Increasingly, organisations are using the framework not only to evidence good practice but to challenge themselves, learn from others, and embed carer partnership more consistently across teams and pathways.
Self-Assessment and Peer Review: What’s Working Well
The self-assessment process continues to be a key entry point for organisations engaging with the Triangle of Care. Where we were updated on how self-assessment encourages teams to pause and reflect on everyday practice, policies, and culture, rather than relying solely on written procedures. When combined with peer review, this reflection is strengthened by external challenge and lived-experience insight.
As part of the update, members were updated on emerging learning from Triangle of Care reports, including self-assessment submissions and peer review feedback. These reports were described as an important source of insight into how carer involvement is experienced on the ground, highlighting both areas of strong practice and recurring challenges across services
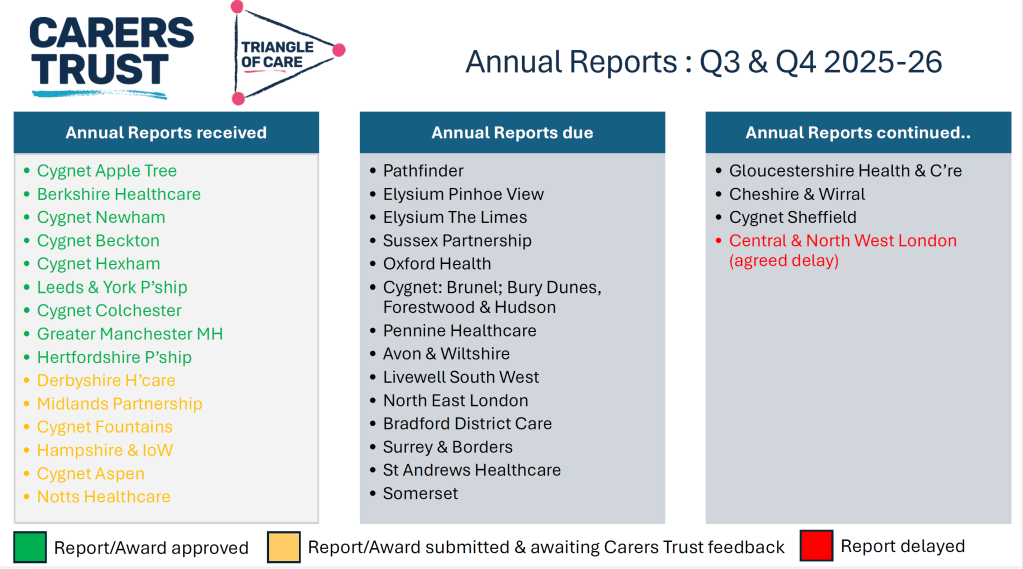
NOTE: These include reports going back 6 months, so not all NHS trusts listed
Peer review was described as most effective when organisations approach it with openness and curiosity. Lived-experience peer reviewers play a crucial role in asking different questions, highlighting blind spots, and grounding discussions in real-world carer experience.
A key discussion point was how to balance national consistency with local flexibility. Members acknowledged that while the Triangle of Care provides a shared framework and standards, services operate within different contexts, populations, and resource constraints.
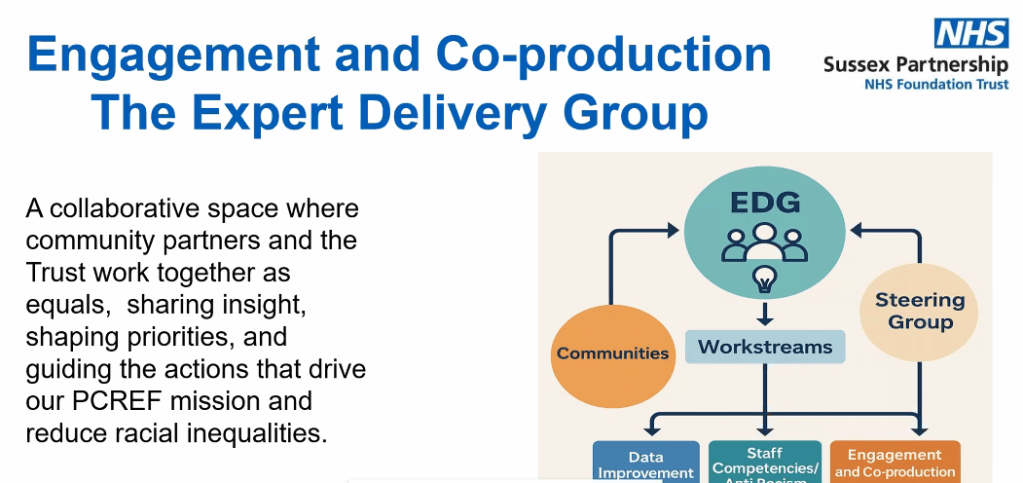
Triangle of care and Patient Carer Race Equality Framework updates
The Triangle of Care and PCREF Phase 2 pilot will be launched in April 2026, to test co-produced specialist guidance to support integration of carers from racially marginalised communities into the Triangle of Care.
Alignment with Wider System Priorities
Members discussed how Triangle of Care activity aligns with broader system developments, including Mental Health Act reform, integrated care, and equality frameworks. There was strong agreement that Triangle of Care should not sit in isolation but be embedded within wider quality improvement, safeguarding, and workforce development agendas.
The need to visibly align Triangle of Care with the Patient and Carer Race Equality Framework was reiterated. Members emphasised that carers must be able to see how equality commitments translate into tangible actions within standards, training, and evidence.
Key points
- Aligning Triangle of Care with Mental Health Act reform
- Embedding within wider system and quality frameworks
- Stronger visibility of equality and race equity
Carer Voice and Evidence of Impact
A recurring theme was the importance of demonstrating impact. Members discussed how services can better evidence carer involvement and experience beyond policies and training records. This includes qualitative feedback, lived-experience insight, and examples of how carer input has influenced service design and delivery.

Emerging Challenges and Areas for Development
The update also acknowledged ongoing challenges, including workforce pressures, digital transformation, and uneven awareness of the Triangle of Care across organisations. Members noted that carer involvement can become fragile during periods of change unless it is firmly embedded in systems and culture.
Summary: Where the Programme Is Heading
The Triangle of Care update concluded with a shared understanding that the programme is well-established but still evolving. The focus for the next phase is on deepening impact, strengthening alignment with equality and legislative change, and supporting services to move from intention to consistent, inclusive practice.
Key discussion points
- Peer review as a developmental, learning-focused process
- Balancing national consistency with local flexibility
- Alignment with Mental Health Act reform and equality frameworks
- Keeping carer voices central to assessment and review
3. Sharing Experiences as a Peer Reviewer
Carer involved with Avon & whitlshire
A carer presented from her involvement at Avon and Wiltshire Mental Health Partnership NHS Trust, where she is involved as a lived-experience peer reviewer contributing to Triangle of Care.
She shared reflections from her role as a lived-experience peer reviewer. She spoke about the importance of authenticity, trust, and transparency in the peer review process, and how lived experience strengthens both credibility and impact. Her contribution reinforced the value of co-production and highlighted how peer review can challenge assumptions, surface good practice, and promote more carer-inclusive cultures within organisations.
The discussion reinforced that organisational openness and leadership engagement are critical to turning peer review feedback into real change. Members reflected on how hearing directly from peer reviewers deepens understanding of the practical impact of policies on carers.
Q&A / Discussion
- Members asked how organisations typically respond to lived-experience feedback.
- The involved carer noted that openness and leadership support were key factors in whether reviews led to meaningful change.
- Discussion reinforced the importance of preparing services for peer review so that carers feel genuinely welcomed and listened to.
4. Carer Contingency Planning – Presentation and Local Practice
Mary Patel
Local example: Carly Driscoll – Bradford District Care
This session focused on carer contingency planning as a key element of carer support and crisis prevention. The presentation outlined why contingency planning is critical in reducing carer anxiety, preventing emergency admissions, and ensuring continuity of care when carers are unable to continue their role.
Carer Contingency Planning (CCP), as championed by Carers Trust, is designed to support carers by planning ahead for times when they might suddenly be unable to continue caring. This might include illness, emergencies, hospitalisation, or other crises. CCP shifts the focus from reactive support during crisis moments to proactive planning that reduces anxiety and prevents avoidable breakdowns in care.
Carers Trust emphasises that CCP is a conversational, personalised process where the carer’s expertise is central. Carers know the routines, preferences, and cues that matter for the person they care for; the goal of CCP is to capture that knowledge in a way that can be shared quickly and effectively with services, families, and emergency responders when needed.
A local practice example from Bradford District Care demonstrated how contingency planning can work in practice, highlighting practical tools, partnership working, and engagement with carers. Discussion explored the benefits of clear, accessible plans, while also acknowledging challenges around awareness, consistency, and uptake

The local practice example demonstrated how contingency planning can be embedded into routine work through partnership approaches and proactive engagement with carers. Members discussed the importance of introducing plans early and reviewing them regularly.
Key features of the Bradford approach
- Routine integration: CCP discussions happen early, not just in crisis moments
- Partnership working: Health, social care, and voluntary sector staff work in concert
- Accessible documentation: Plans are shared in forms that carers can use and update
- Support for carers: Carers are supported to lead the planning, not be passive recipients
- Ongoing review: Plans are revisited as needs and circumstances evolve
Benefits seen locally
- Carers report feeling more confident and less anxious
- Greater clarity across professionals when carers are unavailable
- Fewer last-minute, unplanned crises or service escalations
- Better use of local support networks when official services are stretched
Q&A / Discussion
- Questions focused on how contingency plans are introduced to carers and reviewed over time.
- Members raised concerns about low awareness of contingency planning among carers not already engaged with services.
- Discussion highlighted the need for flexibility, recognising that carers’ circumstances can change rapidly.
5. Carer Contingency Planning – System Perspective
Sara Lewis – SW London ICB
Sara Lewis’s session focused on Carer Contingency Planning (CCP) as a core, preventative element of carer support rather than a reactive or optional add-on. CCP is a structured way of planning for what should happen if a carer is suddenly unable to continue caring due to illness, crisis, exhaustion, or an emergency. At its heart, CCP is about reducing uncertainty and anxiety for carers while ensuring continuity and safety for the person they support.
Sara emphasised that effective CCP recognises carers as partners with expert knowledge of the person they care for. The process supports carers to articulate what matters most, what routines and support are essential, and who needs to be contacted in an emergency. When done well, CCP helps prevent avoidable crises, emergency admissions, and breakdowns in care by making plans visible, accessible, and shared across relevant services.
Accessibility was a major theme, particularly the risks of digital exclusion. While digital tools can be effective, members stressed the need for non-digital options, language support, and culturally appropriate approaches to ensure equity.
Key Takeaways from Sara Lewis’s Session
- Carer Contingency Planning is preventative, not reactive
- CCP is built on early, ongoing conversations with carers
- Plans should reflect what matters to carers and the cared-for person
- CCP must be accessible, inclusive, and culturally appropriate
- Digital tools can help, but must not increase exclusion
- Successful CCP requires shared ownership across services
- When embedded well, CCP reduces crisis, anxiety, and system pressure
Q&A / Discussion
- Members questioned how to balance digital innovation with the risk of digital exclusion.
- Language barriers and accessibility for carers with different communication needs were highlighted.
- Discussion emphasised that contingency planning must be embedded into standard care planning processes, not treated as optional or additional.
6. Looking Ahead: Priorities for the Community Group
The “Looking Ahead” discussion focused on how the Triangle of Care Community Group can continue to influence meaningful change for carers in an evolving policy and practice landscape. Members reflected on the increasing complexity of health and care systems and the importance of ensuring that carers are not left behind as reforms, digital transformation, and workforce pressures accelerate.
A strong theme throughout the discussion was visibility, making carer involvement, equality, and partnership explicit in practice, evidence, and outcomes. Participants emphasised that carers must not only be recognised in principle but experience consistent involvement and support in real-world settings. The group agreed that the next phase of work should strengthen both strategic influence and practical implementation.
Mental Health Act Reform and Carer Involvement

Members discussed the implications of upcoming Mental Health Act reform, particularly around carers’ rights, information-sharing, and involvement in decision-making. There was recognition that Triangle of Care principles provide a strong foundation for supporting services to meet new expectations, but that further work will be needed to translate legislation into everyday practice.
The group highlighted the risk that carers could be inconsistently involved if workforce understanding is weak or if systems focus narrowly on legal compliance. Proactive guidance, training, and examples of good practice were seen as essential to ensure carers are meaningfully included rather than consulted as an afterthought.
Equality, Race Equity, and Inclusion
A central priority looking ahead is ensuring that Triangle of Care activity visibly aligns with the Patient and Carer Race Equality Framework (PCREF). Members stressed that carers from racialised and marginalised communities often face additional barriers to involvement, including mistrust, cultural misunderstandings, and unequal access to support.
The group agreed that equality must be embedded into standards, peer review evidence, and training—not treated as a parallel or optional agenda. This includes capturing meaningful data, listening to diverse carer voices, and ensuring culturally responsive practice is clearly demonstrated.
Workforce Training and Education
Workforce development was identified as a critical lever for long-term change. Members highlighted the need to strengthen carer awareness training across all roles, particularly for staff new to mental health and social care settings. Without this foundation, carer involvement remains inconsistent and dependent on individual attitudes rather than organisational culture.
There was strong support for influencing pre-registration education, including universities and training providers, to embed carer awareness earlier. This was seen as an opportunity to normalise partnership with carers from the start of professional careers rather than trying to retrofit it later.
Key points
- Strengthening carer awareness across the workforce
- Embedding Triangle of Care principles early in training
- Influencing universities and pre-registration pathways
- Moving from individual goodwill to system-wide culture change
Digital, Data, and Accessibility

Digital transformation featured prominently in the discussion, with members acknowledging both its potential and its risks. While improved data systems and digital tools can support information-sharing and coordination, there was concern that carers without digital access or confidence may be excluded.
Participants emphasised that digital solutions must be designed inclusively, with non-digital alternatives always available. Data collection should support understanding of carer experience and inequality, not become a barrier to support.
Key points
- Digital tools should support, not replace, relationships
- Risk of digital exclusion for some carers
- Importance of non-digital alternatives
- Using data to improve equity, not reinforce gaps
Young Carers and Marginalised Groups
Supporting young carers and carers from marginalised communities was highlighted as a continuing priority. Members noted that these groups are often under-identified and less likely to be involved in care planning or decision-making, despite carrying significant caring responsibilities.
The group agreed that future work should focus on visibility, early identification, and tailored approaches that recognise the specific needs and challenges faced by these carers. Partnership with education, community, and voluntary sector organisations was seen as essential.
Key points
- Improving identification of young carers
- Addressing barriers faced by marginalised carers
- Tailored, age-appropriate and culturally sensitive support
- Stronger partnership working beyond health services
Collective Commitment Moving Forward
The discussion concluded with a shared commitment to using the Community Group as a platform for influence, learning, and accountability. Members recognised the value of continuing to share practical examples alongside strategic discussion, ensuring that Triangle of Care principles are translated into everyday practice.
Looking ahead, the group aims to remain proactive, inclusive, and responsive—supporting services to recognise carers as equal partners and ensuring that no carer is left unseen or unsupported as systems evolve.
Key discussion points
- Preparing for Mental Health Act reform
- Embedding the Patient and Carer Race Equality Framework
- Improving workforce training and education pathways
- Supporting young carers and marginalised communities
- Improving data and digital systems without exclusion
As Chair I thanked contributors and reaffirmed the importance of continued collaboration to ensure carers are recognised as equal partners in care, with Triangle of Care principles translated into meaningful practice across services.
For those interested to hear more about triangle of care, see details below