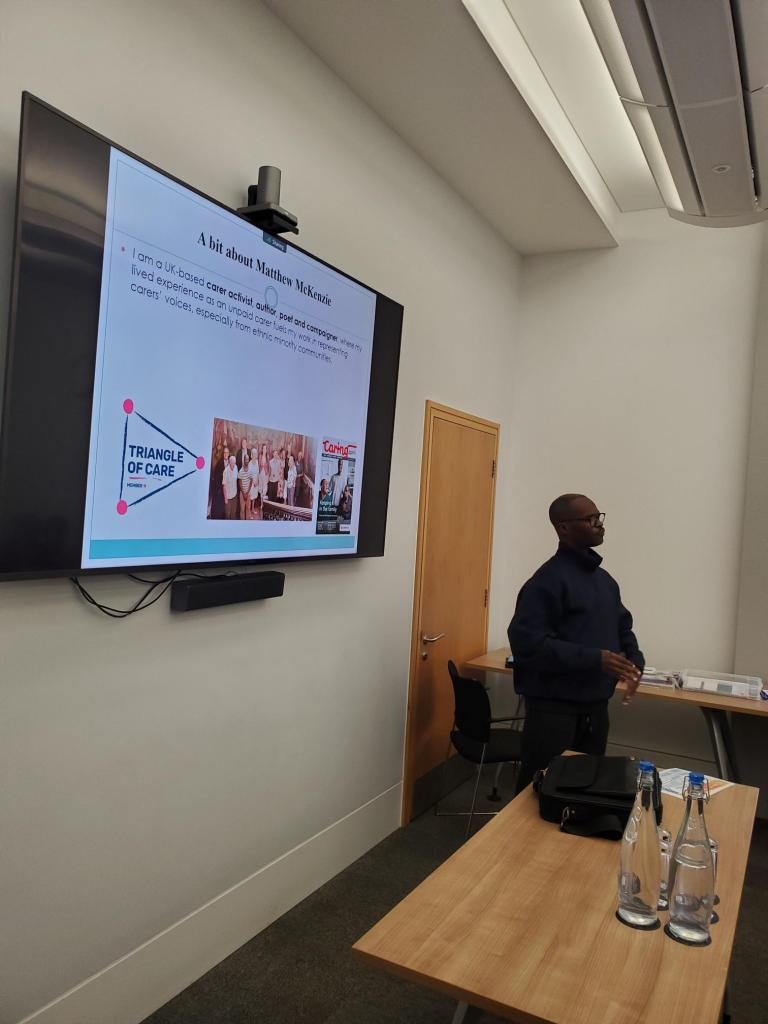
Chaired by: Matthew McKenzie – Lived Experience Carer
Welcome to the November 2025 update of the Hosptial Carer discharge group. The Hospital Carer Discharge Group is a collaborative network chaired by lived-experience carer Matthew McKenzie, bringing together unpaid carers, carer-centre teams, hospital staff and local authority representatives to improve how carers are identified, supported and involved throughout a patient’s hospital journey.
The group provides a space to share updates from hospitals and carers’ organisations, highlight challenges in discharge processes, strengthen links between community and acute services, and promote consistent carer-focused practices such as using the Carers Hospital Discharge Toolkit, developing standard operating procedures, and raising staff awareness.
The November meeting focused updates from the South East London Carer Standard Operating Procedure pilot, improving carer identification, strengthening links between community and hospital services, and practical challenges in engaging hospital teams.
For those who don’t know, In the context of the Hospital Carer Discharge an SOP is a step-by-step, structured process that hospital staff follow to ensure unpaid carers are identified, informed, supported and included consistently during a patient’s hospital stay and discharge.
It usually outlines:
- How to record, communicate and follow up on carer involvement
- Who is responsible at each stage (nurses, discharge teams, carer services)
- What actions must be taken (e.g., asking about caring roles, sharing information, making referrals)
- When these actions should happen (admission, treatment phase, discharge planning)
Who Attended
The session was well attended by a mix of carers, hospital representatives, and carer-centre staff, including:
Carer representatives
- Matthew McKenzie – Chair; lived experience mental health carer; Carers UK, Carers Trust & NHS England Citizens Advisory Group volunteer.
- Caroline – Lewisham carer, Healthwatch Lewisham member & Patient Experience Committee representative.
- Various peer supporters, carers involved in local networks and PPGs.
Carer support organisations
- Carers Hub Lambeth
- Tower Hamlets Carer Centre
- Wandsworth Carer Centre
- North Central London Carers Support Project
Apologies
- Sutton Carers Centre
- Richmond Carers Centre
- Greenwich Carers Centre
- Harrow Carers Centre
- Bromley Well
- IMAGO – Lewisham carers Centre
- Bexley Carers Support
- Involve Kent
Hospitals & NHS staff
- Queen Elizabeth Hospital (Lewisham & Greenwich NHS Trust)
- Public Service Consultants (PSC)
- Bromley, Lambeth, Lewisham, Greenwich council leads (mentioned in discussion)
- St George’s Hospital (GESH) – references to staff
Meeting Overview
- The growing importance of carer involvement in hospitals, especially with mental health pressures and changes to the Mental Health Act.
- The group’s purpose: sharing updates, strengthening links between carers and hospitals, and improving the implementation of the Carers Hospital Discharge Toolkit.
Key Presentation – Update on the South East London Carer SOP Pilot
Speaker: Public Service Consultants (PSC)
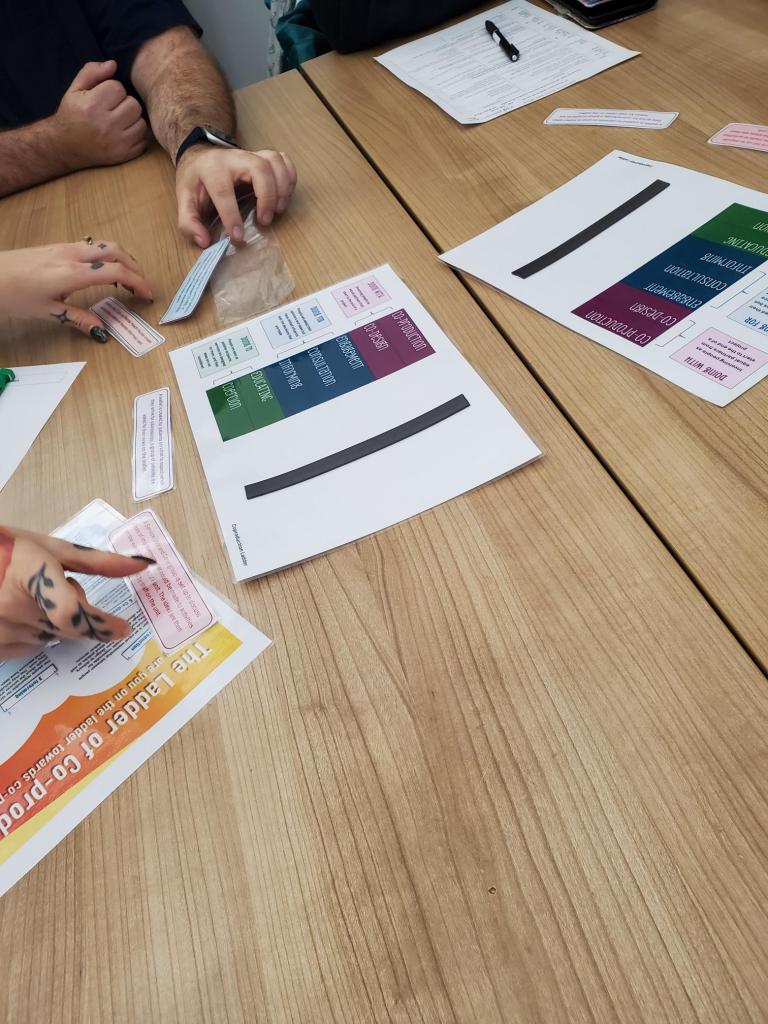
The major portion of the meeting focused on the pilot testing of a new 11-step Standard Operating Procedure for identifying and supporting unpaid carers across hospitals in South East London.
🔹 Hospitals involved in the SOP pilot
- King’s College Hospital – Acute Medicine ward
- University Hospital Lewisham – Hawthorne (older patients) and Alder (specialty medicine) wards
- Princess Royal University Hospital (Bromley) – Frailty Unit via Transfer of Care Hub
🔹 Key outcomes

- King’s College Hospital saw the strongest progress.
- Nurses proactively engaged unpaid carers.
- All leaflets and materials were distributed within weeks.
- Carer details (with consent) were passed to Lambeth Carers Hub.
- Nursing staff requested feedback loops to see the impact of referrals.
- Lewisham Hospital
- Progress slower initially; improved after site visits.
- Ward managers highly supportive and embedding SOP practices.
- Lewisham Council exploring funding for an in-hospital carers support team.
- Princess Royal (Bromley)
- SOP and leaflets now shared with the frailty unit.
- Council to continue taking work forward.
🔹 Overall reflections
- Hospitals still experience heavy winter pressures and staff capacity issues.
- Engagement differs widely between NHS trusts.
- Many ward teams had never seen the London Carers Toolkit, indicating a need for simplification.
- Councils intend to continue cross-borough meetings after PSC’s involvement ends.
Issues & Discussion Points
1. Gaps in consistency across hospital sites
- Queen Elizabeth Hospital (QEH) had not been part of the pilot, they have requested to be included
- Staff expressed interest in adopting SOP materials and joining future rollout.
2. Carer diversity and training needs
Caroline highlighted the need for:
- Training reflecting different care needs: LD, dementia, mental health, elderly carers.
- Cultural diversity considerations in how carers interact with hospital teams.
- Better alignment with Lewisham & Greenwich’s Compassion in Care programme.
3. Current SOP scope limitations
- SOP starts at the ward stage, but carers need involvement pre-admission and post-discharge.
- Best practice from NICE and the national toolkit emphasises whole-journey support.
4. Hospital culture & resistance
Carer-centre staff described feeling:
- Like a “hindrance” in MDT or discharge meetings
- Sometimes unwelcome or blocked from engaging on wards
- Fighting clinical priorities vs. carer rights
- Still needing major awareness-raising to reduce resistance
A carer noted power imbalances and the risk that carers are seen as “barriers to discharge” rather than essential partners.
Updates from Carer Centres & Hospital Teams
Carers Hub Lambeth
- Significant increase in referrals, especially from King’s.
- Engagement seems weaker at Guy’s & St Thomas’, it looks to be still pushing for a stronger carers strategy there, but hopeful the strategy should pick up.
- Working with ward rounds and direct conversations with carers.
North Central London Carers Project

Working across 8 hospital sites, possilbly





- Royal Free Hospital
- Barnet Hospital
- North Middlesex Hospital
- Chase Farm Hospital
- The Whittington Hospital
- University College Hospital
- St Pancras Rehabilitation (Camden and West London)
- Community Central London Trust
- North London Foundation Trust (Mental Health)
Updates include:
- A hospital “menu” to track progress across the toolkit (training, comms, discharge planning).
- Embedding carers into induction programmes.
- Co-authoring discharge documentation at St Pancras Rehab Centre with dedicated “carer sections”.
- Upcoming use of Cerner electronic records system to automatically flag carers.
Tower Hamlets Carer Centre
Carer representative based at Royal London Hospital (east London)

Challenges include:
- Slow referrals & reliance on staff awareness
- Some carers only identified at crisis stage
- Need to expand the carers passport across Royal London
- Hackney pilot ends in March concerns about future funding
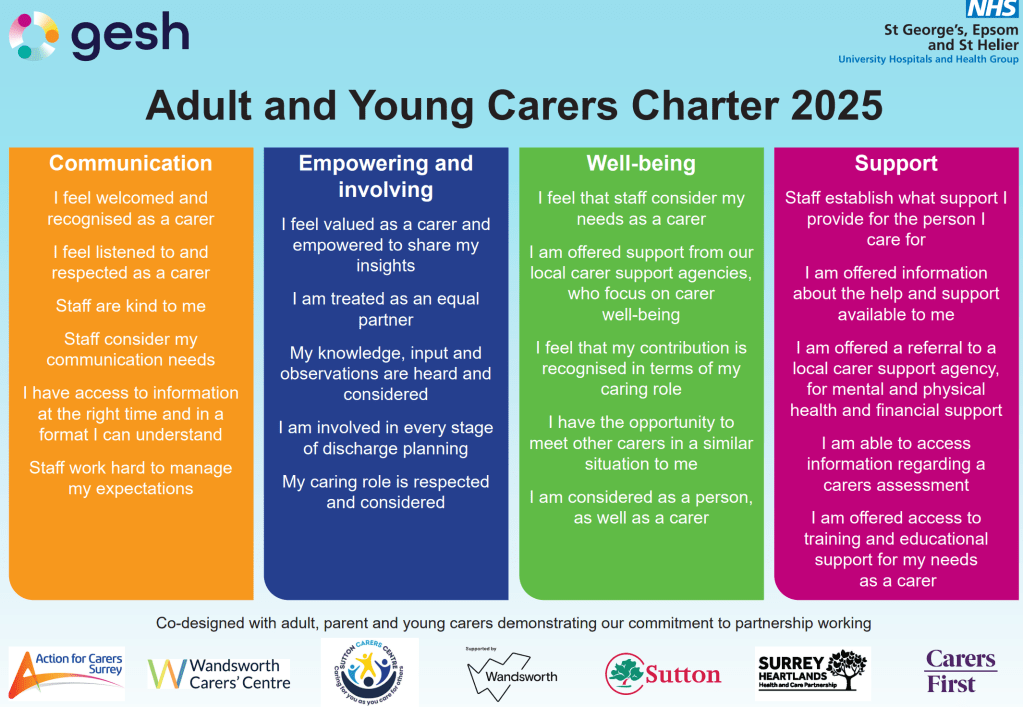
Wandsworth Carer Centre / St George’s

- Developing carer awareness training with Patient Experience Team
- Growth in referrals after training sessions, though staff forget over time
- Plan to expand ward coverage
- As chair I shared St George’s new Carers Charter as a tool for accountability
Carer-Led Developments in Primary Care

A group of Lewisham unpaid carers has begun major work with GP practices, including:
- Creating a PCN-wide carers information pack
- Ensuring carer champions in GP surgeries
- Working with pharmacies to distribute information
- Improving identification on GP systems
- Exploring alignment with Lewisham’s new Carers Action Plan
Plans for the Future
- More invitations to NHS carer strategy leads
- Sharing SOP materials with non-pilot hospitals where possible.
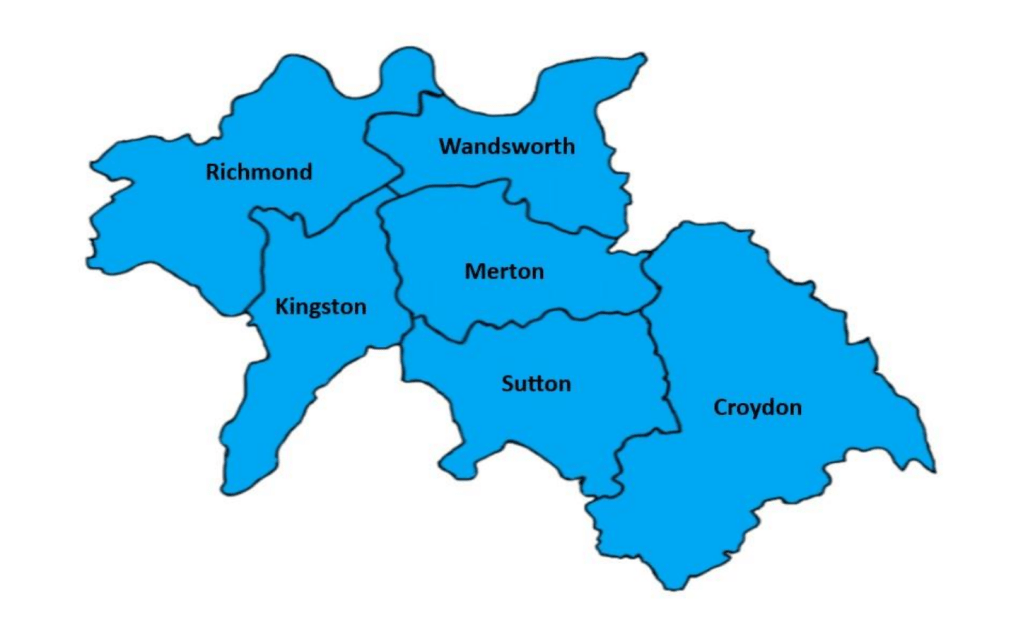
- Matthew to link contacts across councils and hospitals for ongoing monitoring, being the following boroughs e.g.
Lewisham
- Assistant Director – Adult Mental Health & Wellbeing
- Joint Commissioner – Adult Mental Health & Wellbeing
Greenwich
- Strategic Commissioning Lead
- Commissioning Lead for Carers
Bromley
- Assistant Director – Commissioning
- Commissioning Officer
Bexley
- Service Manager – Adult Social Care
Lambeth
- Integrated Commissioning Manager – Adults and Health
Southwark
- Strategic Programmes Manager
- Commissioning Manager
Medium-term aims
- Push for in-hospital carer support teams in Lewisham & Greenwich.
- Expand training and embed carers into staff induction.
- Improve pre-admission and discharge-planning pathways on carer identification and involvement for familes and carers.
- Stronger collaboration between LD nurses, dementia teams, and carers services.
Longer-term aspirations
- Greater consistency across trusts
- Unified carers strategy within each hospital
- A system where carers are routinely recognised, supported, and involved in decisions
Closing Remarks
As cchair I closed the meeting by thanking attendees and acknowledging the collective effort to improve carers’ experiences across London hospitals. I reaffirmed the importance of:
- Making carers visible
- Ensuring rights are upheld
- Strengthening trust–carer relationships
- Carrying learning into the new year
The next meeting will be scheduled in January, with hopes of smoother cross-hospital collaboration in 2024.