brief update By Matthew McKenzie – Chair of the National ethnic mental health carer forum
The January 2026 Ethnic Carer Forum brought together carers, people with lived experience, NHS trusts, community leaders, and national partners to reflect honestly on racial inequalities in health and social care, and to explore how systems can move from good intentions to real change.
The forum continues to act as a safe and challenging space for ethnically diverse and marginalised carers, including Black, Asian, Traveller, LGBTQ+ and other communities, to share experiences, influence policy, and hold organisations to account .
Opening the session, Matthew McKenzie (mental health carer and forum founder) reflected on long-standing inequalities faced by minority carers. He highlighted:
- Persistent mistrust of mental health systems, rooted in lived experience and historical harm
- Patchy engagement by services, despite strong national rhetoric
- Power imbalances that leave carers feeling unheard or excluded
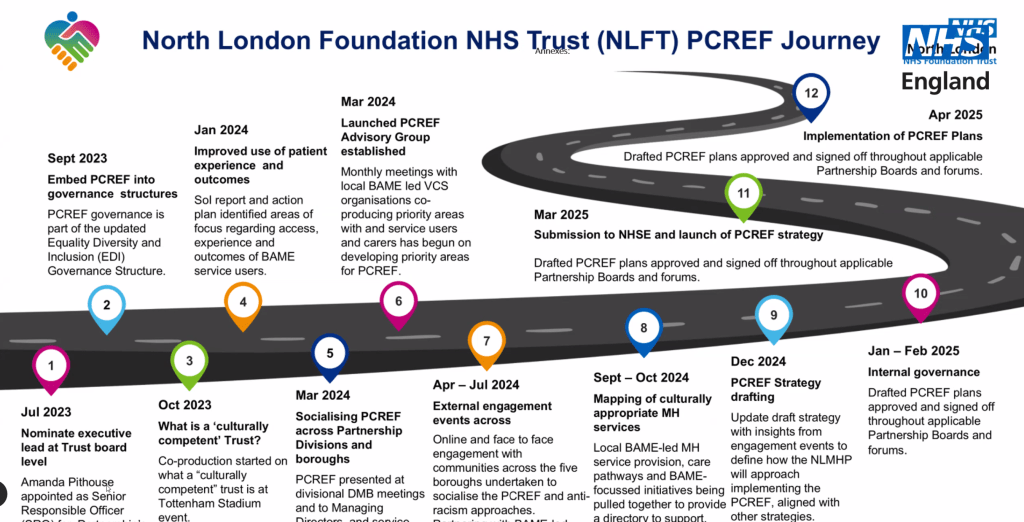
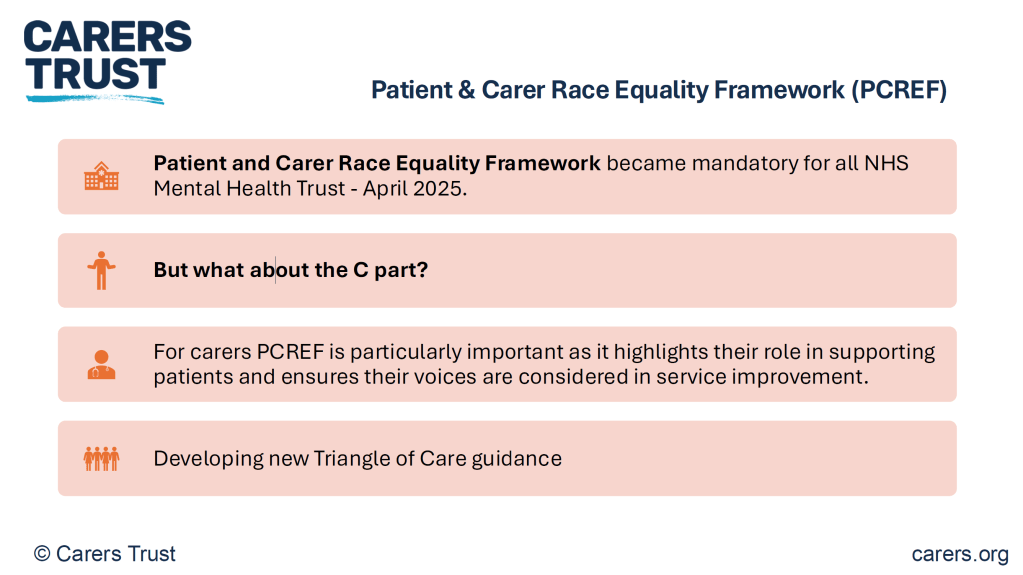
The forum was originally created simply to connect marginalised carers with one another. Today, it also plays a vital role in scrutinising national frameworks, such as the Patient and Carer Race Equality Framework (PCREF), and ensuring carers’ voices shape implementation rather than being added as an afterthought.
Community Voice and National Influence
Race and Health Observatory
Bren, a community volunteer and member of the NHS Race and Health Observatory stakeholder engagement group, shared insights into national efforts to address racial health inequalities.
The NHS Race and Health Observatory: Purpose and Limits
Turning to his national role, Bren explained that the NHS Race and Health Observatory was established in 2021 and funded by the NHS until at least 2027. Its purpose is to:
- Examine racial inequalities affecting both communities and the NHS workforce
- Operate independently, rather than as an internal NHS programme
- Focus on solutions, not just reports and data
He outlined several key areas of current work:
- Small Grants Pilot – supporting community-led initiatives, while acknowledging that funding levels are modest and only a starting point
- Community Participation and Co-production Resource – aimed at helping organisations engage communities more meaningfully and consistently
- Action Resource Platform – an emerging online space intended to bring together data, case studies, and learning in one place

However, Bren was clear that these initiatives are still evolving and must be continuously shaped by lived experience, not institutional convenience.
A Critical Question: Where Are Carers?
One of the most important moments in Bren’s update came when he openly questioned whether carers’ voices are adequately represented within national stakeholder structures including the Observatory itself.

He noted that while there is growing representation from professionals, young people, and community organisations, carers can easily be overlooked unless explicitly prioritised. Bren committed to:
- Reviewing current stakeholder representation
- Raising the absence of carer voices within the Observatory
- Feeding back to the forum on what action is taken
This moment strongly aligned with the forum’s wider purpose: holding national bodies to account while remaining constructively engaged.
Listening as an Act of Power-Sharing
Throughout his update, Bren returned repeatedly to the theme of listening not as a soft skill, but as a deliberate act of power-sharing. He challenged NHS leaders and organisations to move beyond engagement that is performative or extractive.
He stressed that real accountability means:
- Showing communities what has changed as a result of their input
- Being honest when progress is slow or blocked
- Measuring impact through people’s lived experience, not just organisational metrics
As Bren put it, communities do not just want to be consulted they want to see evidence that their voices matter.
Local NHS Action: Gloucestershire Health and Care NHS Foundation Trust
Gloucestershire Health and Care NHS Foundation Trust: Refreshing PCREF with Honesty and Challenge
The update from Gloucestershire Health and Care NHS Foundation Trust offered a candid and important snapshot of what it looks like when an NHS trust acknowledges where progress has stalled and begins the difficult work of rebuilding momentum around race equality and co-production.
Delivered by Ruth, who joined the Trust’s Quality Assurance Directorate in late 2024, the presentation focused on the reinvigoration of the Patient and Carer Race Equality Framework (PCREF) after a period where activity had slowed due to leadership changes and competing pressures.
A central part of the Trust’s renewed PCREF work was a recent Gloucestershire engagement event, which brought together NHS leaders, community members, carers, and national partners to openly explore race inequality, power, and accountability in mental health services.
The event included a powerful contribution from Matthew McKenzie, who presented on how carers should be important to PCREF and the long-term impact this has on trust between services and communities. His contribution was not framed as abstract theory, but rooted in lived experience as a mental health carer and long-standing advocate.
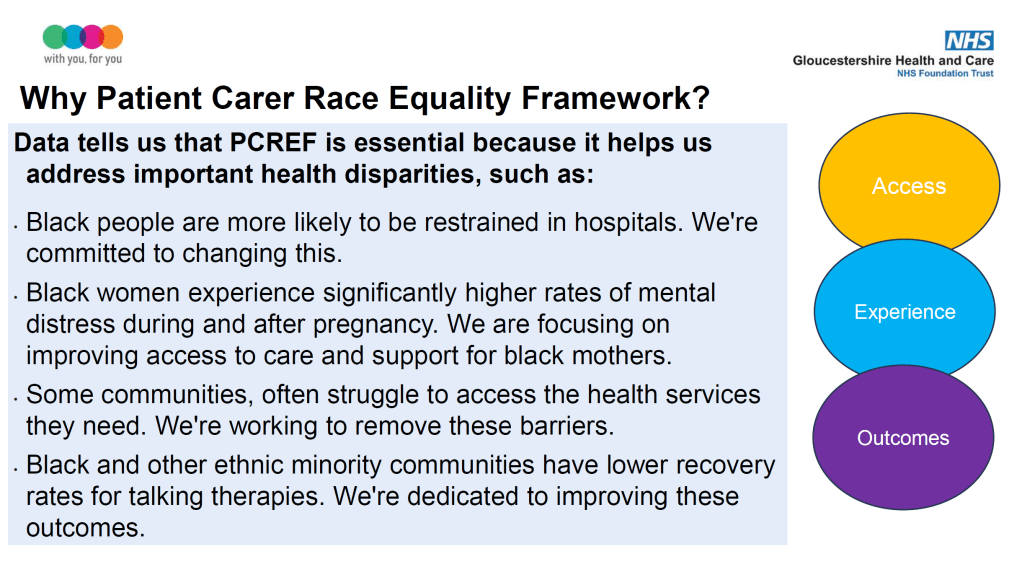
PCREF Matters in Gloucestershire

Ruth began by grounding the discussion in national and local evidence. Despite higher prevalence of mental health need, people from Black and ethnically diverse backgrounds continue to experience:
- Lower access to mental health treatment
- Poorer recovery rates from talking therapies
- Higher likelihood of restrictive practices, including restraint
- Greater mistrust of services, particularly among families and carers
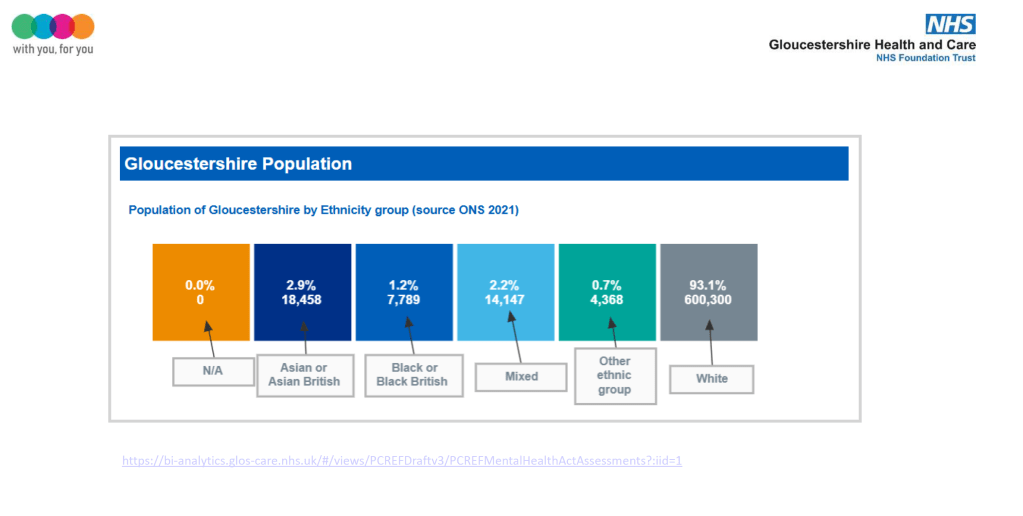
In Gloucestershire, these national patterns sit alongside a population that is predominantly white, which can make racial inequalities easier to overlook or minimise. Ruth was clear that small numbers do not reduce responsibility in fact, they increase the risk that minority experiences become invisible in data and decision-making..
Data: Necessary but Not Sufficient
Data featured heavily in the update and in the discussion that followed. The Trust is working to improve:
- Ethnicity recording, including challenging the routine use of “not known”
- Disaggregation of data on restrictive practices
- Understanding access, experience, and outcomes across services
However, Ruth was clear that data alone does not tell the full story. She spoke about the need to “scratch beneath the surface” and combine quantitative data with lived experience, narrative, and community insight, particularly where numbers are small but impact is significant.
Universal Care Plan (London)
Universal Care Plan (UCP): Promise, Possibility and Carer Challenge
Hayley Blanchard introduced the Universal Care Plan (UCP), currently being rolled out across London as a shared digital record enabling people to document what matters most to them in health and care.
The session on the Universal Care Plan (UCP) was one of the most interactive, challenging, and emotionally charged discussions of the Ethnic Carer Forum. While the tool was presented as a positive step towards personalised and joined-up care, carers and community representatives were clear that digital innovation must not repeat old inequalities in a new format.
The update was delivered by Hayley, a community nurse by background and consultant supporting the UCP programme in London. Her presentation outlined the intention behind the tool but it was the questions from carers that shaped the real substance of the discussion.
What Is the Universal Care Plan?
The Universal Care Plan is a shared digital record, currently available across London, designed to bring together key information about a person’s health, care, and what matters to them all in one place.
The UCP aims to:
- Reduce the need for people to repeat their story to multiple professionals
- Capture personal, cultural, and practical information alongside clinical needs
- Support more joined-up decision-making across services
- Improve coordination in urgent situations (e.g. ambulance or hospital admission)
It is intended for people of all ages and conditions, including those with mental health needs, long-term conditions, and caring responsibilities.
Why the UCP Was Brought to the Forum
Hayley explained that the UCP team is running targeted engagement with ethnically diverse communities, recognising that digital tools often fail those who already experience exclusion, mistrust, or barriers to access.
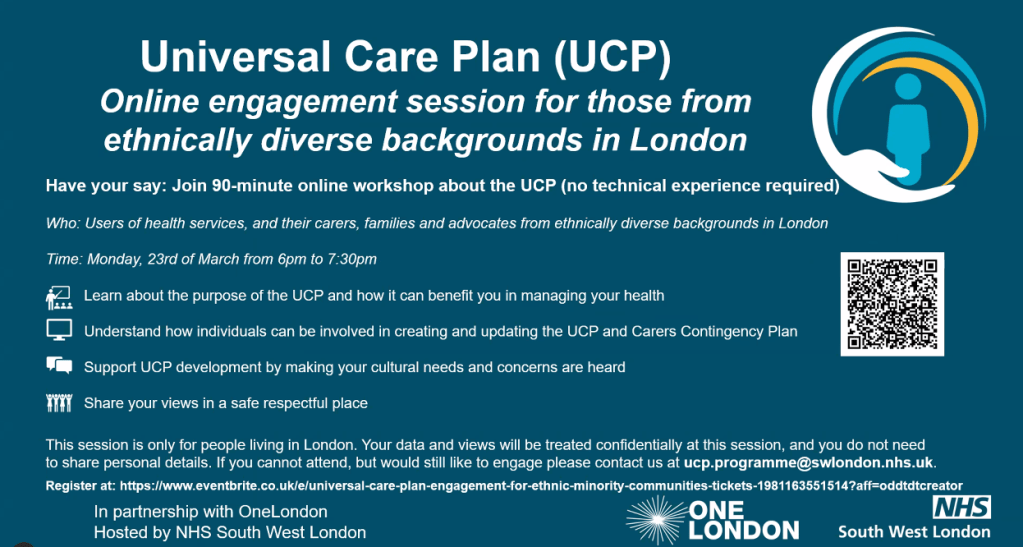
Below You can book for the event to submit your views, its Free to book.
The forum was invited to:
- Scrutinise the UCP from a carer and lived-experience perspective
- Identify cultural, ethical, and safeguarding concerns early
- Influence how the tool develops, rather than responding once it is fully embedded
This framing was welcomed but it did not shield the UCP from robust challenging questions shown below.
1. “Who was this tool designed for clinicians or communities?”
Several carers questioned whether the UCP had been designed primarily from a medical lens, rather than co-produced with people who use services and those who care for them.
2. “Where is co-production and when does it actually start?”
Carers asked whether engagement was happening after development, rather than alongside it.
Key concerns included:
- Whether carers and service users had shaped the structure, language, and assumptions of the UCP
- Whether feedback would lead to real changes, or simply be “noted”
- How communities would know what had changed as a result of their input
3. “What about people who don’t have insight?”
One of the most important safeguarding questions came from carers supporting people with serious mental illness or fluctuating capacity.
Carers asked:
- What happens if someone records decisions that do not reflect their best interests during periods of poor insight?
- How are carers expected to raise concerns if they cannot view or edit the care plan?
- What safeguards exist to prevent harm when information is inaccurate or incomplete?
5. “Who sees this information and where does it go?”
Trust and data sharing were major concerns, particularly for communities with a history of surveillance, discrimination, or misuse of information.
Carers asked directly:
- Which professionals can access the UCP?
- Can information be shared beyond the NHS?
- How is consent managed and reviewed over time?
For some participants, uncertainty around data use undermined confidence in the tool, even if its intentions were positive.
West London NHS Trust: PCREF in Practice
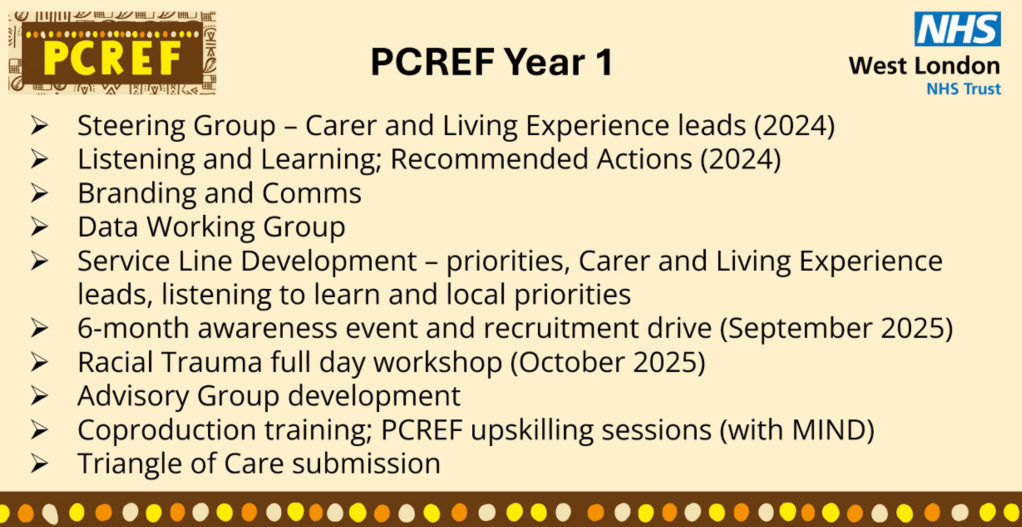
The update from West London NHS Trust offered one of the most honest and grounded reflections of the day on what it actually takes to implement the Patient and Carer Race Equality Framework (PCREF) in a large, complex mental health organisation.
Presented jointly by Linda and pcref carer lead, the update stood out because it did not present PCREF as a finished product. Instead, it described PCREF as ongoing, difficult work, shaped by challenge, learning, and persistence — particularly from carers and people with lived experience.
Building PCREF With Carers and Lived Experience From the Start
Linda explained that West London’s PCREF journey began before her arrival at the Trust, with an intentional decision to embed carers and people with lived experience at leadership level, not just in consultation roles.
From the outset, the Trust established:
- A PCREF steering group with a dedicated carer lead (Debbie)
- A lived experience lead, ensuring parity of voice
- A commitment to co-produce priorities, not simply validate pre-written plans
This early structural choice shaped everything that followed — particularly the Trust’s willingness to sit with discomfort and challenge.
Listening to Learn: Turning Experience Into Action
Throughout 2024, the Trust undertook extensive “listening to learn” work across services. These sessions gathered feedback from carers, patients, and communities about their experiences of mental health care, racism, and exclusion.
Rather than treating this feedback as anecdotal, West London used it to co-produce:
- A PCREF action plan
- Identified priorities for change
- A shared understanding of where harm was occurring — not just where policy said it shouldn’t
This process also highlighted how often data already existed, but had not been meaningfully used or shared.
Data: Knowing the Problem Is Not the Same as Acting on It
West London were open about one of the Trust’s biggest challenges: data transparency and usability.
They acknowledged that:
- The Trust knows Black, African Caribbean and South Asian communities have poorer outcomes and higher drop-out rates, particularly in talking therapies
- Despite this, creating a clear, accessible PCREF dashboard has been slow and frustrating
- Without visible data, communities cannot effectively hold the Trust to account
This honesty resonated strongly with carers, many of whom noted that “knowing the data exists” is not the same as being able to see or use it.
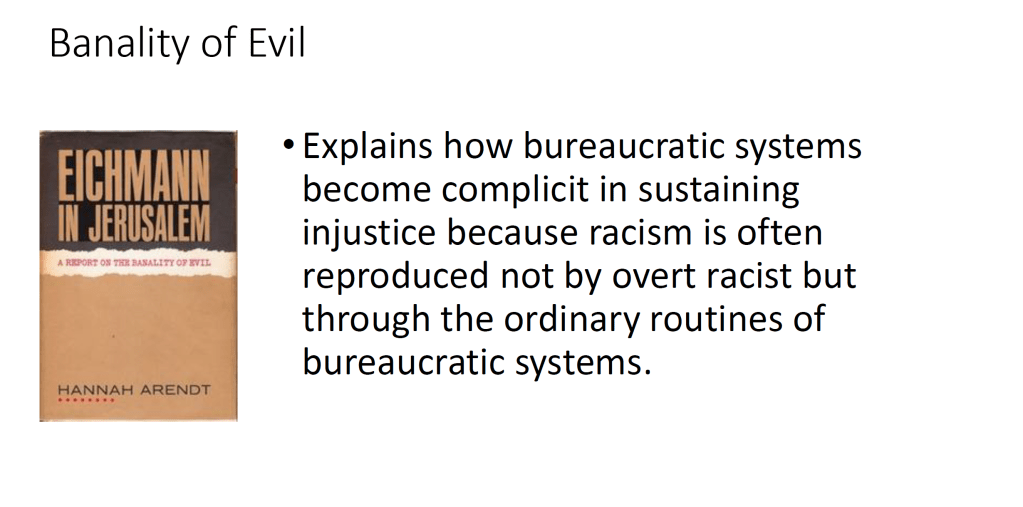
Racial Trauma: Naming the History Behind Mistrust
One of the most powerful elements of the West London update came from the PCREF carer lead account of the racial trauma workshops, which she co-designed and delivered with Linda and colleagues.
These sessions did not begin with policy or frameworks. Instead, they began with history acknowledging the deep roots of mistrust in health systems.
Debbie described how the workshops explored:
- The legacy of slavery and colonial medicine
- Unethical medical experiments on Black and South Asian communities
- How generational trauma shapes present-day interactions with services
Examples such as the Tuskegee experiments and other lesser-known abuses were used not to shock, but to contextualise fear, resistance, and disengagement often labelled as “non-compliance”.
Planning Meaningful Speaker Engagement for 2026
Matthew McKenzie on Shaping the Ethnic Carer Forum Programme
As part of planning for the Ethnic Carer Forum in 2026, Matthew McKenzie presented a structured proposal focused on how speakers and themes should be selected, and why this matters for ethnic minority carers
Matthew explained that the forum’s strength lies in its ability to bring together carers, lived experience voices, community organisations, and systems leaders in a way that feels meaningful rather than tokenistic.
Key Themes Proposed for 2026
Matthew’s presentation outlined 15 proposed themes for the year to invite speakers to the forum for engagement, each linked to clear reasons why they matter to ethnic minority carers. These include:
- Racism and mental health beyond surface-level conversations
- PCREF in practice, focusing on what has actually changed for carers
- Regulation, inspection, and accountability, including complaints processes
- Police involvement, crisis response, and Section 136
- Black mental health and carer experience
- South Asian, Muslim and faith-context carers
- Older adults and intergenerational trauma
- Children, young people, and parent carers
- Carers, poverty, and the benefits system
- Immigration status, NRPF, and mental health
- Co-production: when it works and when it doesn’t
- Workforce racism and its impact on carers
- Alternatives to crisis and coercive care
- Complaints, justice, and redress
- Examples of “what good looks like” — models that have delivered real change
As one participant reflected: “If people can’t see the change, they won’t believe it’s happening