By Matthew McKenzie
I’ve spoken at many events over the years, but standing in a room full of carers always is a great experince differently. The room filled with lived experience, this time paid and unpaid carers carrying invisible weight of caring stories that rarely get space.
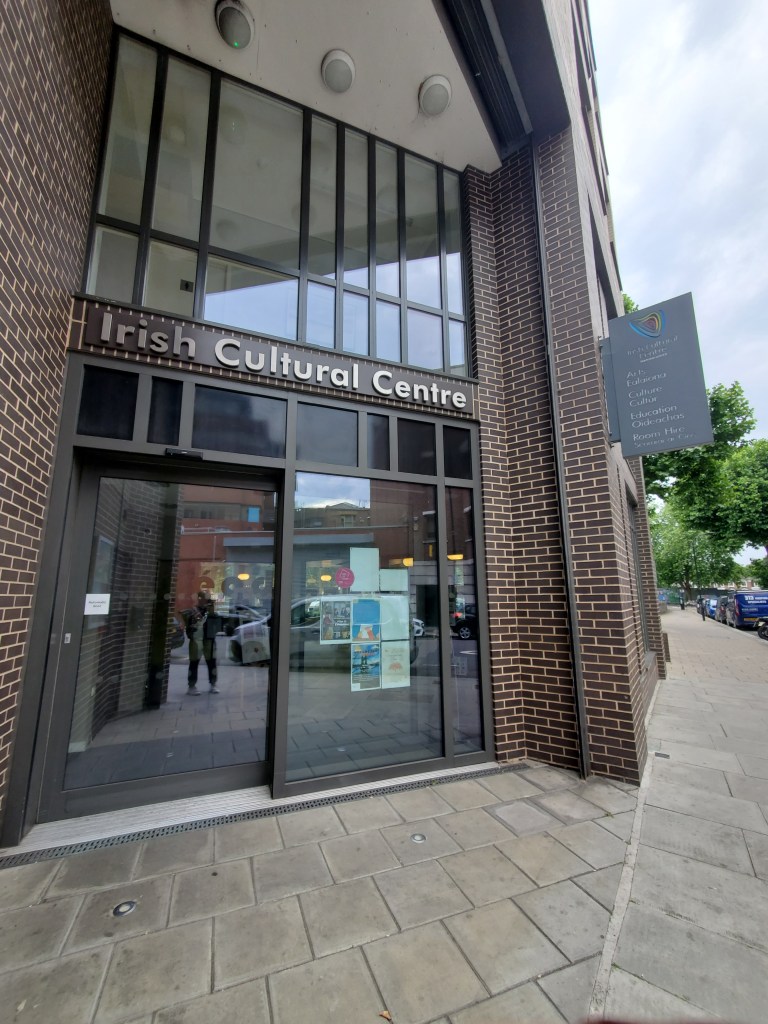
The Carers’ Wellbeing Conference in London, organised by Carers’ Mind CIC, was a moment where carers were allowed to be people first.

The event was hosted at The Abbey Centre, a welcoming community venue in Westminster that provides vital space for local groups, charities, and events focused on wellbeing, inclusion, and social support.
CarersMind CIC is a community-interest organisation dedicated to improving the wellbeing, visibility, and support of both paid and unpaid carers. Through accessible events, practical training, and open conversations about mental health, CarersMind CIC creates safe spaces where carers are recognised as individuals

The Impact of Caring on Mental Health
When I was invited to speak about “The Impact of Caring on Mental Health and What Actually Helps”, I didn’t hesitate. Caring has shaped every part of my adult life. It has taught me empathy, patience, advocacy, but it has also exposed me to burnout, trauma, guilt, and long stretches of isolation.
Too often, carers are spoken about rather than with. This conference made a conscious effort to centre carers’ voices, not as an afterthought, but as expertise.
The Room Told Its Own Story
At the conference, there was no pressure to “cope better” or “be more resilient” without acknowledging the cost. Instead, there was honesty.
Carers spoke about:
- Burnout that creeps in quietly
- Guilt for needing rest
- The emotional toll of long-term responsibility
- Feeling unseen by systems that rely on them
These were truths that deserved to be heard without judgement.
What Claire Shelton Shared at her session
Claire spoke openly about how caring impacts mental health carers over time, not just during moments of crisis. she talked about trauma that doesn’t announce itself, about stress containers that overflow slowly, and about how carers often normalise distress because “there’s no other option.”
Most importantly, she focused on what actually helps:
- Being recognised as a carer both formally and emotionally
- Access to peer support, not just professional services
- Practical tools that reduce isolation
- Boundaries that protect carers’ wellbeing without guilt
One resource Claire highlighted was the Hub of Hope, because carers need access to support that doesn’t require jumping through endless hoops. These matter not because they fix everything, but because they return a small amount of control to people who’ve lost a lot of it.
What I Shared in my session
In my session, I spoke from lived experience about the long-term impact of caring, shaped deeply by my role as a carer for my mother. I shared how caring is rarely defined by single moments of crisis, but by the gradual, cumulative pressure that builds over time. This includes the emotional labour, the constant vigilance, and the way stress and trauma often go unrecognised because caring simply becomes “what you do.”

I reflected on how caring for my mother affected my mental health, identity, and sense of self. This experience led me to speak about carers’ rights the right to be recognised as a carer, to be involved in decisions, to access support, and to protect one’s own wellbeing without guilt or fear of judgement.
Most importantly, I focused on what actually helps:
- Being identified and recognised as a carer, both formally and emotionally
- Understanding and exercising carers’ rights
- Access to peer support grounded in shared lived experience, not only professional services
- Practical tools that reduce isolation and complexity
The Power of Being in the Same Room
One of the most powerful moments wasn’t during my talk it was during the conversations that followed. Carers sharing strategies with each other. Nodding in recognition. Saying, “I thought it was just me.”
That’s the quiet power of events like this. They remind carers that their experiences are valid, shared, and worthy of space.
A Collective Effort

It was a privilege to share the day with:
- Claire Shelton, who spoke with clarity and compassion about resilience, stress management, and boundaries
- Klivert Jabea, who brought warmth, insight, and a strong message that self-care is not a luxury
- The organisers at Carers’ Mind CIC, who created an environment that felt safe, inclusive, and genuinely carer-focused
This conference was about acknowledging reality and that’s where real wellbeing work begins.
Leaving with Hope and Responsibility
I left the Abbey Centre reminded of why this work matters. Carers are holding together families, communities, and systems often at great personal cost. Supporting carers isn’t optional. It’s essential.
Resources and Support for Carers
If you are a carer and are looking for support for your wellbeing, mental health, or caring role, the following resources were highlighted or reflected in discussions during the conference:
- Hub of Hope — https://hubofhope.co.uk
A free, UK-wide mental health support database that helps carers find local and national services quickly, without needing to navigate complex systems. It is particularly useful for carers who may not know where to start or who feel overwhelmed by traditional referral pathways. - CarersMind CIC — https://carersmind.co.uk/
A community interest company focused on improving carers’ mental health and wellbeing through events, training, and open conversations that centre lived experience. Their work creates spaces where carers feel recognised, heard, and supported. - Carers UK — https://www.carersuk.org/
Provides information on carers’ rights, benefits, assessments, and practical guidance for unpaid carers across the UK. - Mind — https://www.mind.org.uk/information-support/helping-someone-else/carers-friends-family-coping-support/
Offers mental health information, helplines, and local services, including support relevant to carers experiencing stress, anxiety, or burnout. - NHS Carers Support
Local NHS and local authority carers services can offer carers’ assessments, signposting, and practical support. Availability varies by area, but carers have a right to request an assessment. - Rethink Mental Illness – Carers Hub — https://www.rethink.org/advice-and-information/carers-hub/
- Information and guidance for carers supporting someone with mental illness, including rights and practical support.