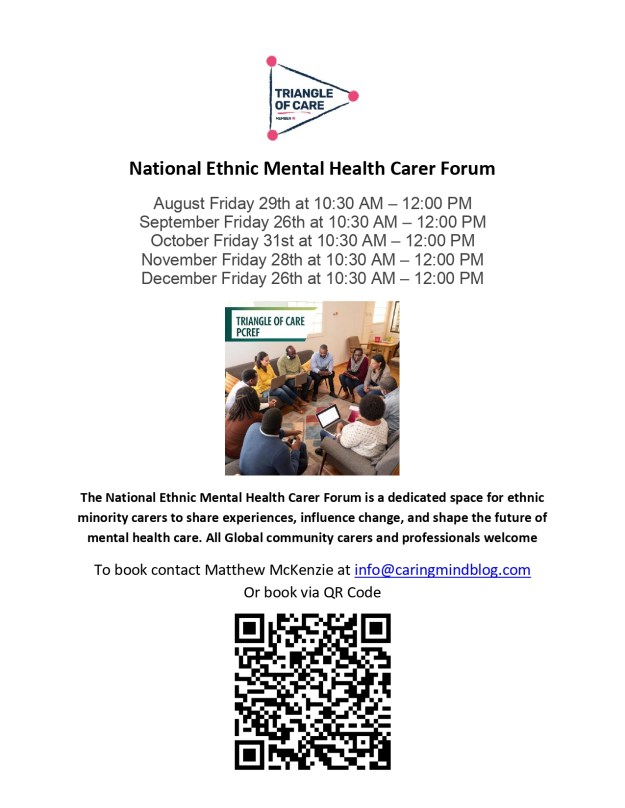
by Matthew McKenzie – National Ethnic Mental Health Carer Forum Chair
In August, the online National Ethnic Mental Health Carer Forum came together once again to confront difficult but necessary conversations about systemic racism, discrimination, and the experiences of ethnic minority carers within health and social care. The forum, hosted by Matthew McKenzie, provided a platform for carers, professionals, and researchers to share insights, frustrations, and plans for change.
Focus on Racism and Discrimination
This month’s forum was unflinching in its focus: racism in health and mental health systems. Attendees shared powerful testimonies of racial abuse and discrimination, highlighting how these experiences undermine trust in services and affect both carers and those they support. There was a clear call for honesty – participants stressed the importance of naming racism directly, rather than disguising it behind euphemisms.
The group also discussed the overrepresentation of Black and brown people in prisons, the lack of tailored initiatives for older Black carers, and the persistent inequalities faced by ethnic minority families trying to navigate mental health and social care support.
Research and Evidence from Carers Trust
A key presentation came from Andrew of Carers Trust, who shared research into the barriers faced by Black, Asian, and minoritised ethnic carers. The findings highlighted widespread issues: discrimination, language barriers, lack of cultural competence, and difficulties in accessing benefits. Andrew emphasised the need for culturally inclusive services and stronger outreach strategies, while acknowledging feedback from the forum that research and advocacy must be explicit about racism rather than avoiding the term.
Andrew expanded on the importance of equity in benefit advice, pointing out that many carers miss out on their entitlements because information is inaccessible, overly complex, or not communicated in culturally relevant ways. He called for dedicated advice services that are not only multilingual but also sensitive to carers who may not self-identify as such.
He also spoke about the impact of social isolation on carers from ethnic minority backgrounds, who often have fewer support networks and face stigma within their own communities. Addressing this requires building trust with local organisations and ensuring carer support is visible in spaces where communities already gather, such as faith centres or community hubs.
Finally, Andrew outlined the Carers Trust’s national strategy, which involves working more closely with local carer organisations, producing research that amplifies marginalised voices, and lobbying for systemic reforms. He highlighted how this forum’s feedback directly shapes their advocacy, showing a real commitment to partnership.
Questions raised during Carers Trust’s presentation:
- How can Carers Trust ensure its research explicitly names racism rather than using softer language?
- What specific support can be offered to carers who do not self-identify as carers and miss out on benefits?
- How can Carers Trust improve its complaints handling processes, particularly for carers facing racism and discrimination?
- What role can MPs and lobbying groups play in supporting Carers Trust’s advocacy for ethnic minority carers?
- How will Carers Trust ensure its multilingual materials are distributed widely enough to reach isolated communities?
Hampshire & Isle of Wight NHS Anti-Racism Initiatives
Usually NHS Mental Health trust representatives update on anti-racism initiatives at the forum. This time Hampshire and Isle of Wight engaged with minority carers.
Elton who is the Diversity and Inclusion Partner from Hampshire and Isle of Wight NHS Trust provided an update on their anti-racist programmes, including the rollout of the Patient and Carer Race Equality Framework (PCREF). The trust has begun implementing cultural competence training, engaging with local communities, and embedding anti-racism into its wider mental health services. While early in its journey, the trust is already seeing changes in communication and engagement across different wards and services.
Elton shared that the trust is actively developing training modules on implicit bias, with the aim of reaching every staff member across its services. This training is intended not as a one-off exercise but as part of a sustained culture change programme. Early feedback from staff has been encouraging, with more frontline workers recognising how unconscious bias can influence treatment decisions.
He also described the trust’s efforts to engage directly with service users and carers, ensuring that their lived experiences feed into decision-making. Listening events, surveys, and advisory panels are being used to capture diverse perspectives, with a particular focus on groups who historically felt excluded from consultation.
In addition, Elton emphasised the need for transparency and accountability. The trust will publish regular updates on its PCREF action plan, allowing communities and stakeholders to scrutinise progress. He acknowledged that this is just the beginning, but stressed that embedding anti-racism into healthcare systems requires openness, humility, and sustained commitment.
Participants raised questions about how these initiatives address specific groups, such as older Black carers and prisoners’ families, as well as concerns about public misconceptions of anti-racism work. Elton acknowledged these challenges and committed to following up with colleagues on gaps raised during the discussion.
Questions raised during NHS Trust’s presentation:
- How will PCREF specifically address the needs of older Black adults who often feel invisible in services?
- What is being done to support the mental health of prisoners (e.g. Albany and Parkhurst prisons) and their families within this anti-racist framework?
- How will the trust prevent the public misconception that PCREF “excludes” white people?
- What mechanisms are in place to ensure transparency and accountability in publishing progress updates?
- How will the trust measure the long-term impact of cultural competence and implicit bias training?
Academic Research Contributions
The forum also heard from Shylet, a PhD researcher from University of Glasgow, who is focusing on learning disabilities. She presented her work on the lived experiences of Black African families caring for adults with learning disabilities, and invited participants to take part in interviews. Their contributions highlighted the importance of academic research in documenting and amplifying carers’ lived realities.
For more details you can contact her at S.Musabayana.1@research.gla.ac.uk
Carers’ Experiences of Benefits and Support
Another important theme was the financial challenges facing carers. The group discussed the complexity of benefits like Carer’s Allowance and how misinformation or fear of losing other entitlements often deters carers from claiming support. A carer expressed reluctance to claim due to concerns about how it might affect their relative’s benefits, while another highlighted the importance of valuing one’s own contribution and recognising caring work. There was frustration with bureaucratic systems that seem designed to exclude, particularly when layered with the additional barriers of language, culture, and discrimination.
Carers also highlighted the immense value of unpaid care, with estimates placing its worth at over £180 billion per year if it were to be paid for by the NHS. This figure underscored the urgent need for better recognition and support of carers’ contributions.
Strengthening Complaints and Accountability
There was a debate around how carers can raise complaints when faced with racism or poor treatment. Many participants expressed a lack of trust in formal systems like the CQC or Ombudsman, feeling that complaints disappear into bureaucracy without change. Suggestions included working with MPs, lobbying groups, or the media to ensure voices are heard.
Final Reflections
The August forum showed once again how necessary it is to hold these difficult conversations. Carers spoke bravely about racism and exclusion, professionals shared updates on anti-racist strategies, and researchers sought to bring lived experience into policy. Yet the message was clear: systemic change requires more than frameworks and research reports. It requires honesty, collaboration, and persistence.
As host, I was encouraged by the passion and determination in the room. The forum continues to grow as a national voice for ethnic minority carers, and our commitment to addressing racism head-on remains at the heart of this work.