By Matthew McKenzie – TOC Community Chair
Our final Triangle of Care (ToC) Community Group meeting of the year brought together carers, professionals, and ToC members from across the UK to share updates, raise concerns, and discuss priorities for 2026 and beyond. Although Microsoft Teams provided some surprises, we made it work, thanks to teamwork and patience. The conversation was rich, heartfelt, and often very moving.

1. Opening & Agenda
As chair of the meeting, I acknowledged technical teething problems as the group used Teams for the first time in this format. Mary (ToC Programme Lead) welcomed attendees and explained the privacy-driven decision to hide email addresses, which also unfortunately hid attendees’ names. A fix will be implemented before the January meeting.
The agenda included:
- Triangle of Care national updates (Mary)
- Carer co-production and lived experience input (Matthew)
- Surrey & Borders’ co-production example (postponed)
- Research priority-setting presentation (Richard, University of Manchester)
- Carer questions and discussion
2. Triangle of Care National Update (Mary)
Mary provided a comprehensive end-of-year update structured around ToC’s three priority areas for 2024–25.

2.1 Embedding the Relaunched Triangle of Care Framework
Growth & progress
- 16 new members have joined the scheme since April, bringing ToC membership to over 80.
- The first Welsh hospital achieved a ToC Star Award, prompting the creation of a new Welsh-language logo and Welsh materials.
- A social care pilot is underway with Livewell South West, with West Hertfordshire Teaching Hospital reviewing ToC criteria for an acute setting.
- Nine Star Awards have been achieved this year, with a further 12 annual reviews approved. Many more annual reports are pending review before year-end.
Standardising data
Mary emphasised the push for consistent reporting across Trusts, including:
- numbers of carers identified
- uptake of carer awareness training
- numbers of carer champions
This will help build a national picture of impact.
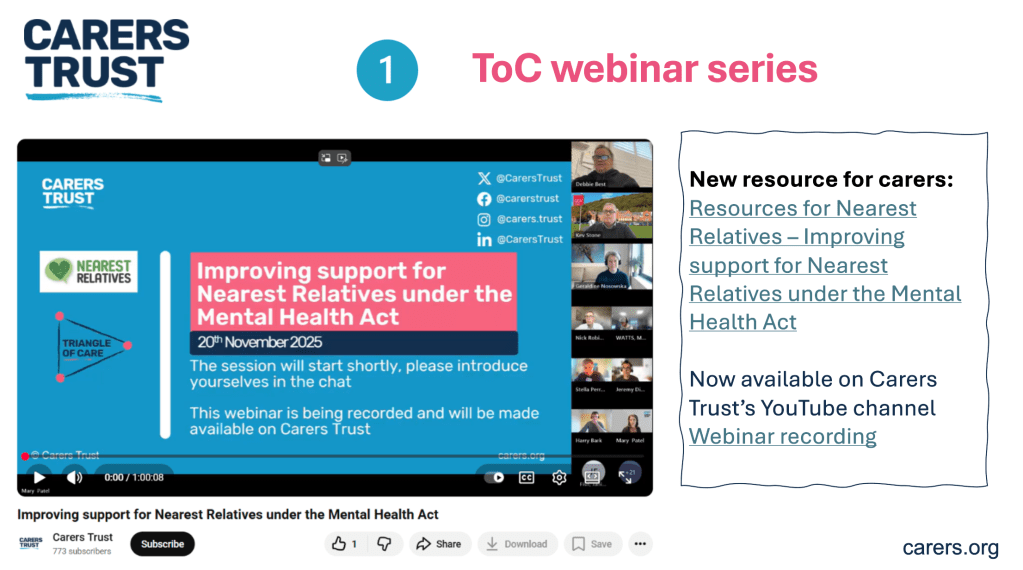
Webinars
ToC’s Lunch & Learn series continues, with the recent Carers Rights Day webinar (in partnership with University of Bristol) focusing on the Nearest Relative role under the Mental Health Act (MHA). Resources are available via Carers Trust’s YouTube channel.
2.2 Young Carers: Identification & Support
A major update was the successful national policy win relating to young carers and the Mental Health Act.
Mental Health Act Reform – Safety Net for Young Carers
Following campaigning by Carers Trust, the Young Carers Alliance, and ToC members who wrote to MPs:
- Government has agreed to update the MHA Code of Practice to require:
- identification of children when an adult is detained
- sharing of information about available support
- referrals for young carer needs assessments
- Updates to advance choice documents will require practitioners to ask about dependent children.
- Expected implementation: Summer 2026.
This win was warmly welcomed by the group.
2.3 Racially Minoritised Carers & PCREF
Mary updated members on ToC’s work to ensure carers are fully represented in the Patient & Carer Race Equality Framework (PCREF).
Key updates
- A national Task & Finish Group has now completed its review of the first four ToC standards; the final standard is underway.
- Piloting of new culturally sensitive criteria is planned with 10 NHS Trusts beginning April 2026.
- Example of early good practice: Livewell South West is implementing a new “essential data template” that includes carers, enabling services to better identify and support racially minoritised carers.
- Carers Trust is calling for a statutory duty for NHS mental health providers to implement PCREF in full, including community governance.
2.4 Changing the Narrative on Care – New Research
Mary introduced new research (supported by the Health Foundation and Oxfam GB) titled Changing the Narrative on Care, highlighting:
- Although 80% of the public value unpaid care, this does not translate into policy action or investment.
- Three recommended reframes:
- Care is a universal experience, not a niche issue.
- No care without support, make support visible and tangible.
- Care is a partnership between families, communities and systems—not something families must do alone.
The full report is available on Carers Trust’s website.
3. Carer Involvement, Co-Production & Lived Experience (Matthew McKenzie)

I then presented an in-depth reflection on the value of authentic carer involvement, drawing on his lived experience and his role working with multiple NHS organisations.
Key points included:
- Carers are not passive observers, they hold critical lived knowledge that improves services.
- Real co-production goes beyond consultation; carers must be equal partners in shaping policy, documentation, training, and strategic decisions.
- Examples Matthew gave from his own involvement:
- redesigning welcome packs and leaflets
- addressing confidentiality misapplication
- involvement in recruitment panels
- delivering training to staff at induction
- reviewing complaints and compliments themes
- advising on discharge processes and family-inclusive safety protocols
- participating in research steering groups
- Carers’ insight is especially essential in safeguarding, quality boards, and identifying service gaps often invisible to professionals.
4. Surrey & Borders Co-Production Example
A planned presentation from Surrey & Borders was postponed, as the relevant colleague could not attend with materials. They hope to present at a future meeting.
5. Research Priority Setting in Secure & Forensic Mental Health (Richard Kears)
Richard introduced a national project with the James Lind Alliance (JLA) aiming to identify the top 10 research priorities for secure and forensic mental health services across England, Scotland and Wales.
Who is the survey for?
- Carers
- People with lived experience of secure/forensic services
- Staff working in these services
- Anyone indirectly connected (victims, families)
Purpose
To ensure future mental health research is led by the real concerns of those most affected, not only by academics or pharmaceutical interests.
Process
- National survey gathering research questions.
- Analysis to identify common themes.
- Second, more focused survey to refine priorities.
- National workshops with carers, staff and people with lived experience to finalise the top 10.
A QR code and flyer were shared for distribution. The group expressed strong support.
6. Attendee Discussion & Questions
This was the richest section of the meeting, with many heartfelt contributions. The themes below reflect the key concerns raised.
6.1 Scotland & UK-wide ToC Alignment
A carer asked why Scotland’s ToC framework is separate and not integrated into the UK ToC accreditation model.
Mary explained:
- Scotland currently uses ToC only as a free policy framework.
- Implementing the accreditation model in Scotland would require groundwork to assess willingness and ability of providers to fund membership.
- Integration is being discussed but is not imminent.
6.2 Clarity on Co-Production
Several carers voiced concerns that:
- “Co-production” is often used as a buzzword.
- Some NHS Trusts label work as co-produced after completing it.
- Carers need clarity on what ToC means when using the term.
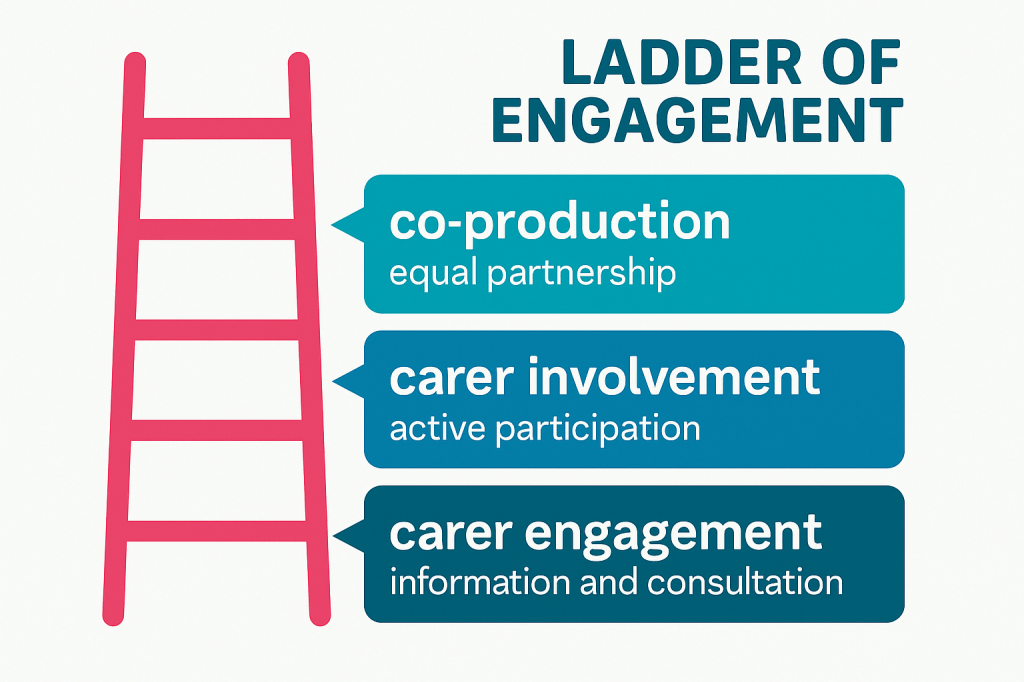
Mary responded that ToC uses a ladder of engagement, distinguishing:
- carer engagement
- carer involvement
- full co-production
Carers Trust is developing a formal principles-based statement on involvement for future meetings.
6.3 Older Carers: Visibility, Support & Inequalities
The majority of carer questions focused on the unmet needs of older adult carers, many of whom are supporting people with severe mental illness—not dementia—and often have been caring 20–40 years.
Attendees reported:
- Feeling “invisible” within both policy and services.
- Being incorrectly grouped under “older carers = dementia”.
- Their own poor health affecting their caring ability.
- Increasing struggle to get responses from professionals.
- Serious concerns about who will care for their loved ones when they die.
- Feeling less heard as they age, compared with younger carers or newer voices.
One carer (age 78) shared:
“I can’t retire from caring. Benefits stop at 65, but the caring doesn’t.”
Another said:
“We have to shout louder as older women to be heard—and still we aren’t.”
Mary acknowledged the seriousness of these issues and committed to:
- bringing older carers’ concerns into ongoing ToC work
- exploring dedicated guidance and better mainstreaming within the ToC standards
- sharing good practice on carer contingency planning in upcoming meetings
I have placed the guide below
I also reiterated the group’s role in surfacing policy gaps and influencing future national lobbying.
6.4 Carer Registration & Meeting Access
Several carers raised issues with:
- The length of the ToC sign-up form
- Not receiving meeting links despite signing up
- Verification barriers when joining Teams
Mary agreed to:
- review and shorten the form
- clarify which fields are optional
- address email deliverability issues
- adjust MS Teams settings to reduce joining friction while maintaining security
6.5 Concerns About Confidentiality Misuse
One carer reported that in a CQC meeting at an NHS Trust, raising questions about communication was dismissed as “confidentiality”, preventing meaningful dialogue.
I then encouraged carers to bring such examples into:
- ToC Star peer reviews
- Carer involvement forums
- Local advocacy routes
He noted that misuse of confidentiality is a common and unacceptable barrier and must be challenged.
6.6 Petition on Antipsychotic Medication Research
Carers highlighted concerns about:
- long-term prescribing of antipsychotics
- lack of regular medication review
- inadequate research into long-term effects
A carer shared a petition calling for investigation of psychiatric medications. Richard noted that he had signed and shared it previously.
7. Closing Remarks
Matthew thanked all attendees for their honesty, passion and persistence:
“Carers’ voices shape policies and improve care. That is exactly what this group is here to do.”
Mary acknowledged:
- the importance of every concern raised
- the need to better support older carers
- improvements to ToC communications and meeting accessibility
- that the next meeting will be in January (provisionally 19th)
The meeting closed with gratitude from carers who said they felt heard, supported, and connected.