By Matthew McKenzie
On 25th February 2026, I had the privilege of speaking at the Carers’ Forum hosted by Involve Kent.
Involve is a voluntary sector infrastructure organisation in Kent that supports unpaid carers by providing information, advice and practical help to make caring more manageable.

They organise regular carers’ forums and events where carers can meet each other, access specialist support services, hear from guest speakers on issues like benefits, legal rights and wellbeing, and contribute their lived experience to local planning and decision-making. Involve also connects carers with tailored resources, signposts to relevant services across health, social care and community sectors, and advocates for carers’ voices to be heard by policymakers and service providers
The forum ran from 10:30am to 1:30pm and brought together unpaid carers from across Kent to connect, learn and have their voices heard.

It was my second time speaking at this forum, and once again I was struck by something powerful: the room was full. That might sound simple, but in the world of unpaid caring which can often feel isolating and invisible a full room means solidarity. It means people are choosing, despite exhaustion and competing demands, to show up for themselves and each other.
Arriving and the atmosphere
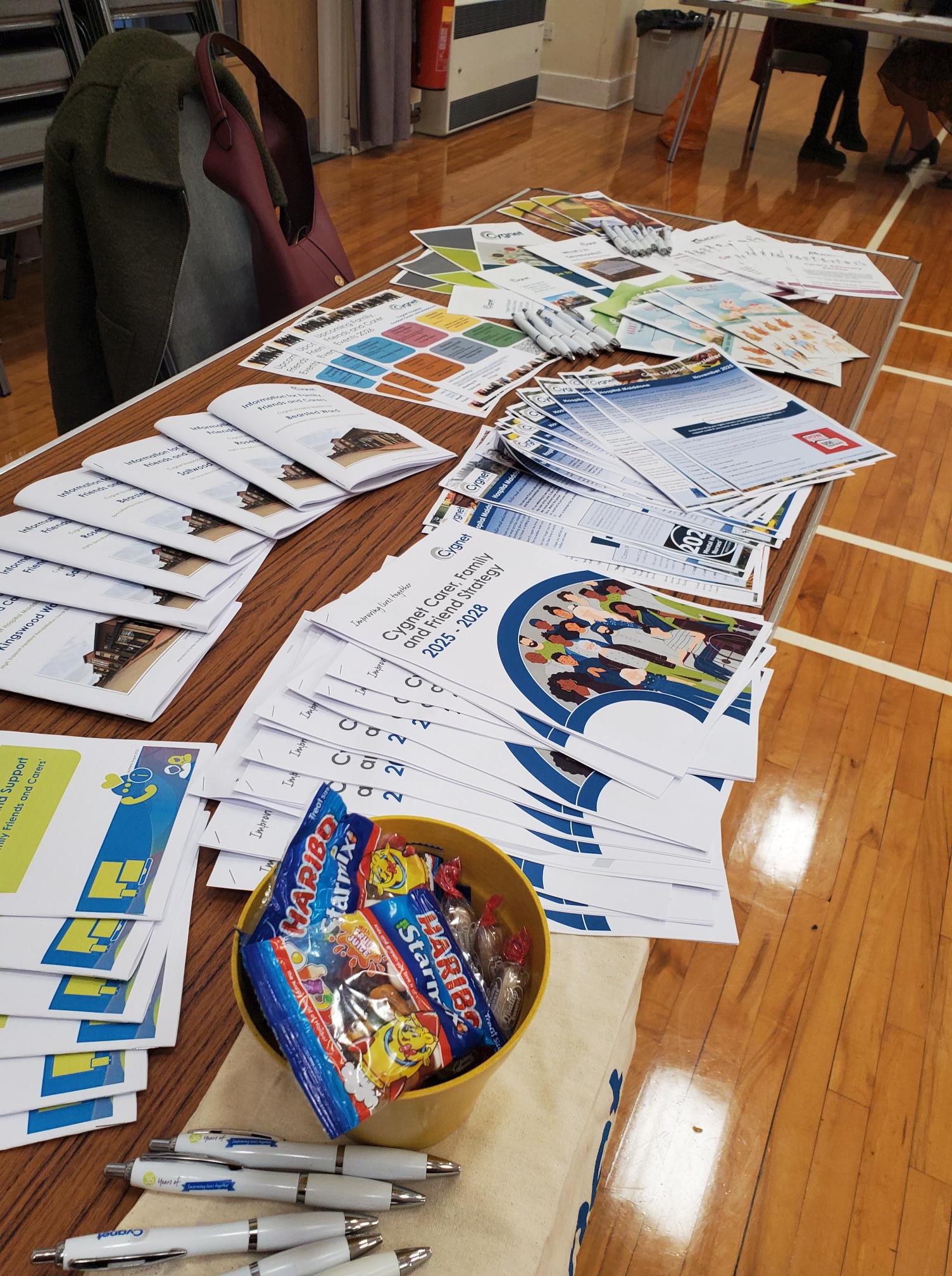
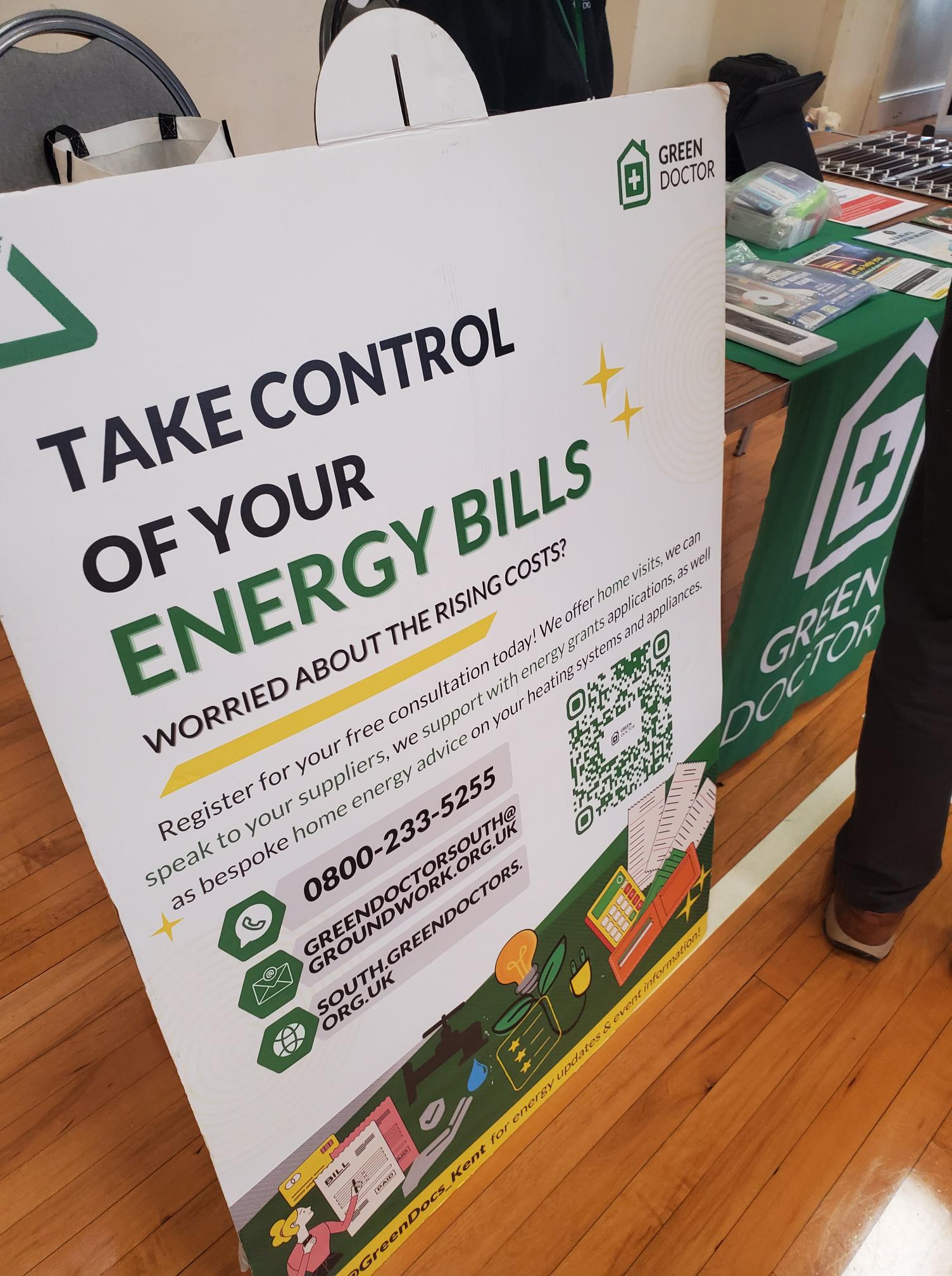
From the moment I walked in, there was a real sense of warmth. Information stands lined the hall Involve, Citizens Advice, mental health services, energy advice, leisure services and more. Tables were covered in leaflets, conversations were already flowing, and carers were reconnecting with familiar faces.




The purpose of the forum was clear:
To enable those caring unpaid for an adult family member, partner or friend to meet, gain information about services in their community and have their voices heard .
That last part to have their voices heard is what resonated most with me.
It was also good to see Carer leads from Cygnet Maidstone engaging with carers in the community of Kent.

My talk: Caring for someone with a mental health diagnosis
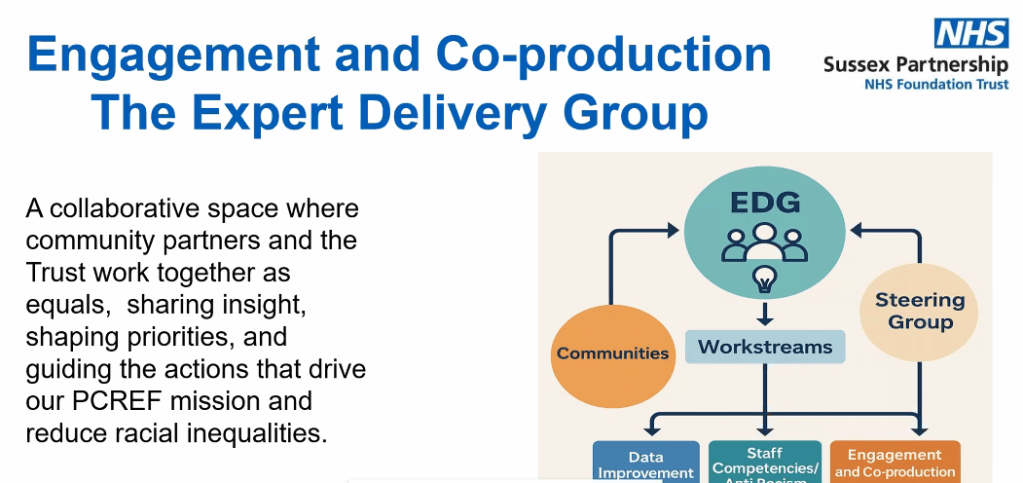
I spoke about caring for someone with a mental health diagnosis and the Patient and Carer Race Equality Framework .

As many know, I cared for my mother who lived with schizophrenia, and I now support a close friend who lives with personality disorder and addiction challenges. I don’t speak as a clinician. I spoke as someone who has sat in GP waiting rooms, on inpatient wards, in crisis meetings, and at home during those “screaming silences” that carers know too well.
I shared:
- The confusion I felt when I didn’t even realise I was a “carer”
- The frustration of confidentiality barriers
- The loneliness of not being listened to
- The emotional exhaustion that comes from constantly firefighting crises
I then shared a poem to promote carers rights
But I also shared something equally important: growth, advocacy and solidarity.
I encouraged carers to:
- Educate themselves about the condition they are supporting
- Learn the difference between symptoms and personality
- Understand triggers
- Forgive themselves for mistakes
- And most importantly, look after their own wellbeing
One message I always return to was – You cannot pour from an empty cup.
I also spoke about The Patient Carer Race Equality Framework
It exists because there is clear evidence of:
- Disproportionate detentions under the Mental Health Act
- Poorer outcomes for Black and minority ethnic patients
- Higher levels of distrust between communities and services
- Carers feeling unheard or excluded
I spoke about how minority carers can face:
- Cultural misunderstandings
- Language barriers
- Stigma around mental health within communities
- Fear of services due to past discrimination
- A lack of culturally appropriate support
Discussion tables: Carers influencing change

After my talk, Clara from Involve led discussions feeding into Kent’s Health Needs Assessment for carers. Carers were asked:
- How do you recognise when it’s time to ask for help?
- What causes burnout?
- What would a carer-friendly community look like?
These wete not token questions. Staff took notes (without identifying details) so carers’ lived experiences could directly inform local planning .
I moved around the room speaking with carers. Some were open and vocal. Others were quieter, but their listening was just as powerful. Not everyone wants to speak publicly and that’s okay. Being present is also participation too.
Power of Attorney – protecting your voice
Later in the morning, Glen Miles spoke about the Mental Capacity Act and Lasting Power of Attorney .

As carers, we often assume we will automatically be consulted in crises. The reality is different. Without legal authority, our ability to advocate can be limited.
One key takeaway:
- Don’t delay in arranging Lasting Powers of Attorney.
- If you want your voice – or your loved one’s voice – to be heard, formalise it.
For carers who have experienced being excluded from decisions, this was a particularly important session.
Citizens Advice & practical support
Ian from Citizens Advice spoke before lunch about benefits, debt, housing and confidential support .
With the cost of living crisis, carers are under immense financial pressure. Many reduce employment hours or leave work entirely. The session was a reminder that:
- Advice is free
- It is confidential
- You can attend anonymously
- You are not judged
Lunch followed – catered by Fusion – and honestly, some of the most meaningful conversations happen over sandwiches. Carers swapping stories. Sharing phone numbers. Recommending services. That peer-to-peer support is priceless.


What stayed with me
What stayed with me most wasn’t just the agenda or the presentations.
It was:
- The older carer quietly nodding as I spoke about emotional exhaustion.
- The new carer asking, “Is it normal to feel this angry sometimes?”
- The male carers who stayed behind to speak to me privately.
- The carers from minority backgrounds who spoke about cultural barriers and stigma.
These forums matter because carers matter.

Unpaid carers save the system billions. But beyond economics, we hold families together. We absorb crises. We advocate in rooms where we’re not always welcomed.
Involve Kent (Carers’ Support – West Kent)
Address:
30 Turkey Court, Turkey Mill, Ashford Road, Maidstone, Kent, ME14 5PP
Telephone: 03000 810 005
General email: hello@involvekent.org.uk
Carers support contact: communitynavigation@involvekent.org.uk
Website: http://www.involvekent.org.uk