By Matthew McKenzie – A Caring Mind
If you’re an unpaid carer in Southwark, chances are you’re used to putting everyone else first. You support a loved one day in, day out, emotionally, practically, often invisibly. And too often, decisions about “support” for carers are made without carers truly being heard.

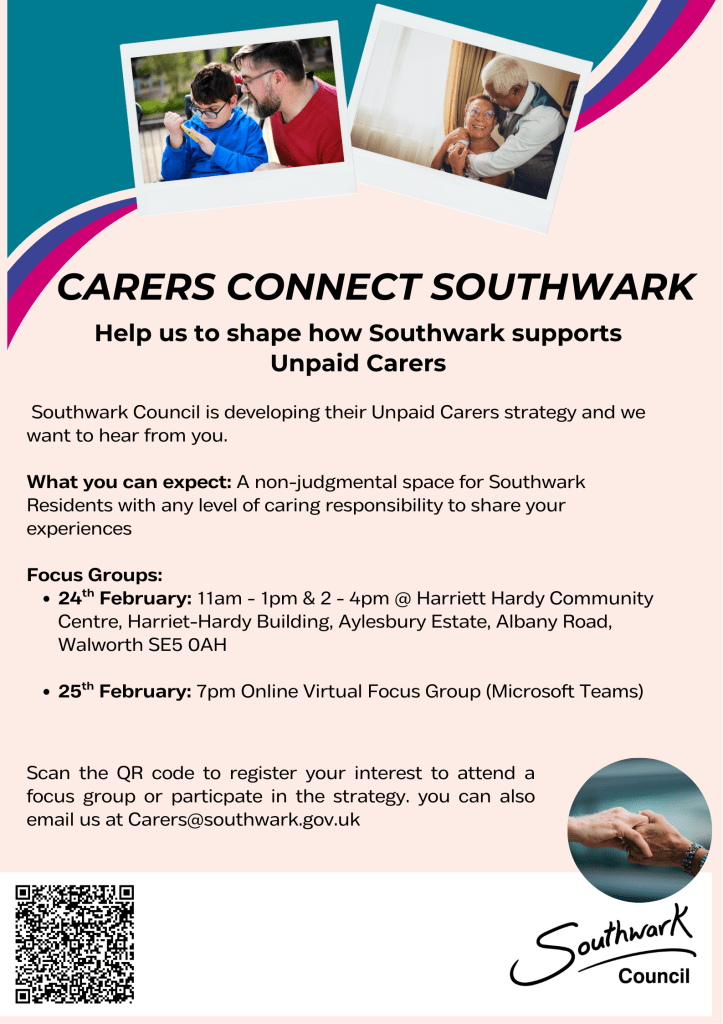
Southwark Council is developing its Unpaid Carers Strategy, and they are inviting unpaid carers to take part in upcoming focus groups to share real experiences, which are your lived reality.
As an unpaid carer myself, I know how rare and valuable this opportunity is.
Why having your say is important because
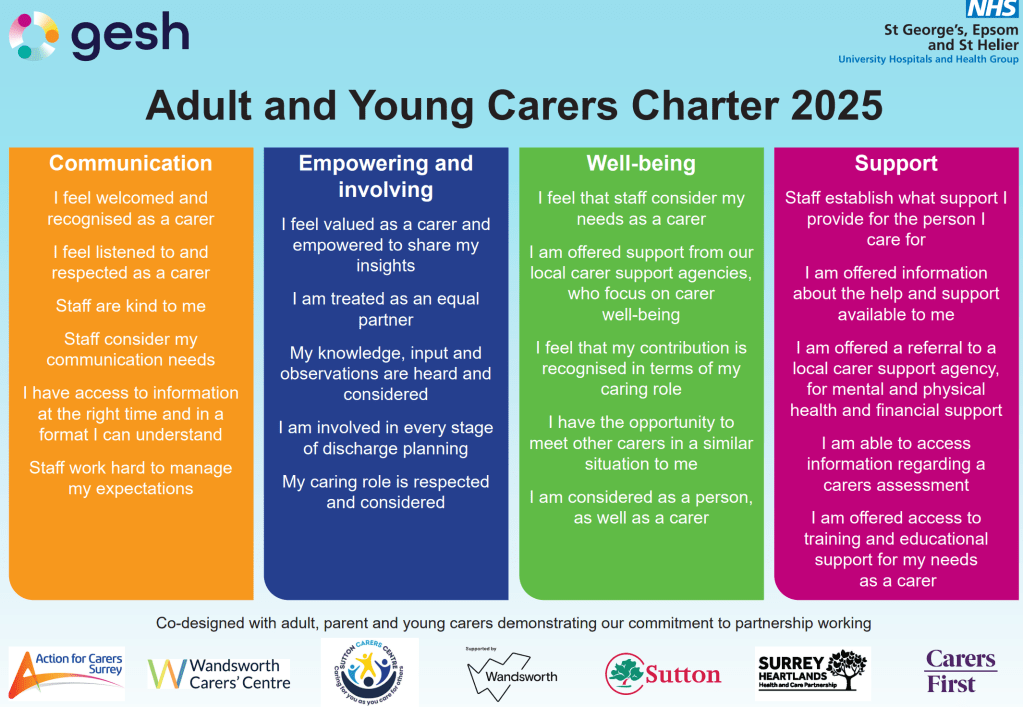
Policies and strategies shape:
- What support is available
- How easy (or hard) it is to access help
- Whether carers feel recognised, supported, and understood
When carers don’t speak up, systems are built around us, not with us. When we do speak up, its a chance to make change becomes possible.
This isn’t about complaining.
It’s about being honest: what works, what doesn’t, and what would genuinely make life easier for carers in Southwark.
Your voice could help shape:
- Better access to information and services
- More flexible, carer-friendly support
- A strategy that reflects the real pressures carers face
A safe, non-judgemental space
One of the most important things about these focus groups is that they are designed to be:
- Non-judgemental
- Inclusive
- Open to carers with any level of responsibility
You don’t need to have all the answers.
You don’t need to be an “expert”.
You just need your experience.
Whether you care full-time, part-time, occasionally, or don’t even label yourself as a “carer” your perspective still counts.

Focus group dates and details
In-person focus groups
📅 24th February
⏰ 11am – 1pm and 2pm – 4pm
📍 Harriet Hardy Community Centre
Harriet-Hardy Building, Aylesbury Estate, Albany Road, Walworth SE5 0AH
Online focus group
📅 25th February
⏰ 7pm
💻 Virtual session via Microsoft Teams
How to get involved
You can:
- Scan the QR code on the flyer shown above my blog to register your interest
- Or email Carers@southwark.gov.uk
Even attending one session can make a difference — not just for you, but for other carers now and in the future.
A personal note from me
As unpaid carers, we are often exhausted, overlooked, and expected to “just cope”. Opportunities like this don’t come around often.