By Matthew McKenzie
As the NHS looks to the future with its ambitious 10-Year Plan, one critical group continues to be overlooked cancer carers, although I am not forgetting Mental Health carers. These are the unpaid family members, friends, and loved ones who provide essential care and emotional support to people living with cancer.

While the plan addresses key priorities like digitalization and community-based health reform, it fails to fully recognize the vital role of caregivers in our healthcare ecosystem.
The blog is a transcript of my video, which you can watch below.
Reform Through Inclusion
The NHS 10-Year Plan aims to reshape health services by emphasizing digital tools, preventive care, and stronger local networks.

These initiatives are undoubtedly important. But without recognizing and integrating the contributions of cancer caregivers, the plan risks missing a vital component of patient care.
The Invisible Workforce
Caregivers are often the unsung heroes of cancer care. They manage appointments, administer medications, provide emotional support, and serve as advocates all while coping with their own mental and physical toll.
Challenges Faced by Cancer Carers:
- Mental Health Impacts: The stress, anxiety, and emotional burden can be overwhelming.
- Decision Fatigue: Carers are often thrust into complex medical decision-making without adequate support or guidance.
- Lack of Recognition: Despite their contributions, caregivers are rarely acknowledged as part of the healthcare team.
A Call for Systemic Change
The inclusion of carers in healthcare reform isn’t just an ethical necessity it’s a strategic imperative. By empowering carers, we enhance patient outcomes, reduce strain on NHS services, and promote more holistic care.
Recommendations for Inclusion:
- Training for Carers: Equip caregivers with tools to better navigate health systems and support patient needs.
- Support Services: Invest in respite care, mental health support, and caregiver-specific community services.
- Recognition in Policy: Classify caregivers as essential stakeholders in healthcare planning and delivery.
Co-Production: Designing Services With Carers
One of the most powerful messages from the discussion is the importance of co-production. That means actively involving carers in designing and shaping NHS services not just consulting them after the fact.
Co-Production Actions:
- Involve Carers in Service Design: Make caregiver feedback a routine part of NHS planning.
- Policy Advocacy: Push for legal and procedural reforms that recognize the role of carers from day one.
The Road Ahead
Cancer caregivers are not just a support system they are key partners in the healthcare journey. If the NHS truly seeks to build a more inclusive, responsive, and sustainable health system, caregivers must be central to its 10-Year Plan.
Let’s stop treating caregivers as an afterthought. Let’s make them co-creators of the future of care.
Support Sites for Cancer Carers
1. Carers UK
Provides advice, online forums, factsheets, and rights information for unpaid carers across the UK.
https://www.carersuk.org
2. Carers Trust
Supports a network of local carer organisations across the UK. Offers practical help, grants, and local service finders.
https://www.carers.org
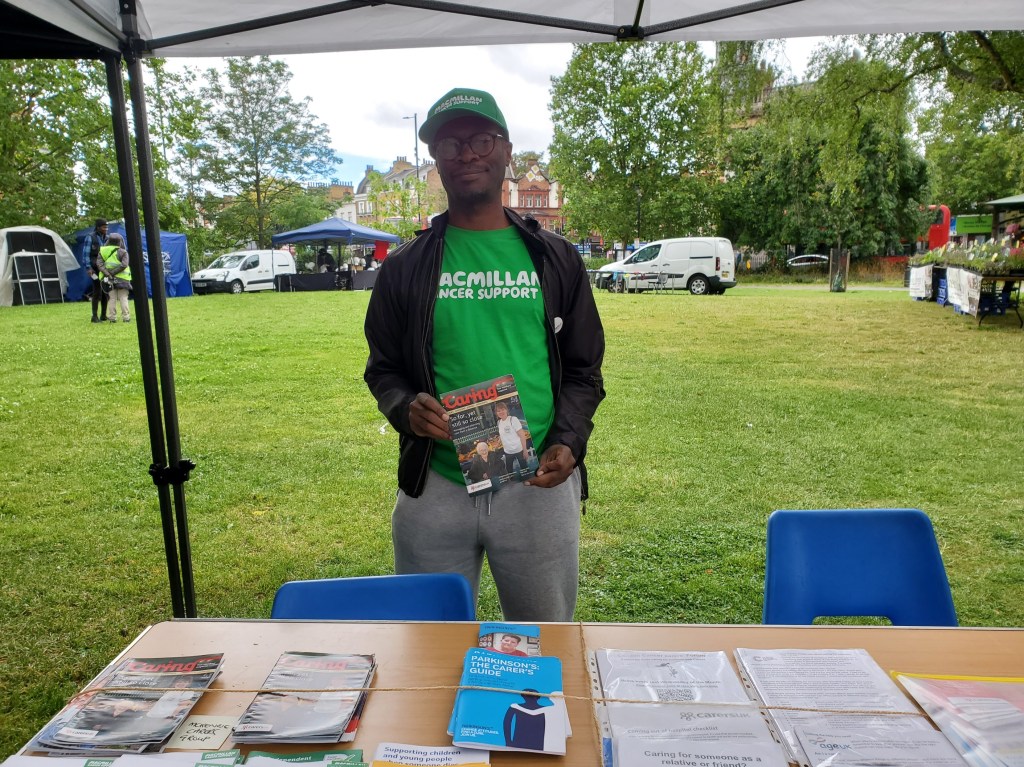
3. Macmillan Cancer Support
Offers emotional, practical, and financial support for people affected by cancer—including dedicated resources for carers.
https://www.macmillan.org.uk/information-and-support/supporting-someone-with-cancer
4. NHS – Cancer Care and Support
Official NHS guidance on cancer, treatments, living with cancer, and how carers can support loved ones.
https://www.nhs.uk/conditions/cancer/
5. Maggie’s Centres
A network of cancer support centres offering free emotional, psychological, and practical support to anyone affected by cancer—including carers.
https://www.maggies.org
6. Marie Curie – Caring for Someone with Cancer
Offers support to those caring for someone at the end of life or with a terminal cancer diagnosis, including bereavement help.
https://www.mariecurie.org.uk/help/support/caring