The meeting facilitated by Matthew McKenzie began with introductions from participants and updates on various carer support initiatives, including forum mergers and NHS plan changes.
Local council strategies and initiatives were discussed across different boroughs, with particular focus on Lambeth and Southwark’s carer support plans and the development of a carer’s forum in Lewisham. The group explored challenges faced by carers, including access to primary care and the need for better coordination, while discussing recent conferences and upcoming events aimed at supporting and advocating for carers’ rights.
Lewisham Carers Strategy and Service Updates

Lewisham is currently refreshing its Carers Strategy to strengthen support for unpaid carers and improve access to local services. The focus is on ensuring carers are included in decision-making through co-production and collaboration with the council, health providers, and community organisations. A major priority is improving well-being services, providing better information, and ensuring carers know their rights under the Carers Leave Act.
As part of wider NHS reforms, Lewisham is moving towards a neighbourhood-based care model designed to bring services closer to local communities. While this aims to make access more seamless, carers raised concerns about inconsistent GP access, gaps in communication, and challenges navigating between boroughs when supporting loved ones. The forum highlighted the importance of better coordination between primary care, hospital discharge planning, and mental health services to ensure carers are recognised and supported.
Lambeth Carers Strategy Refresh

Lambeth is currently refreshing its Carers Strategy with the aim of improving services, increasing visibility, and ensuring carers have a stronger voice in decision-making. The updated strategy focuses on key priorities such as well-being, access to assessments, respite options, and workforce training for those supporting unpaid carers.
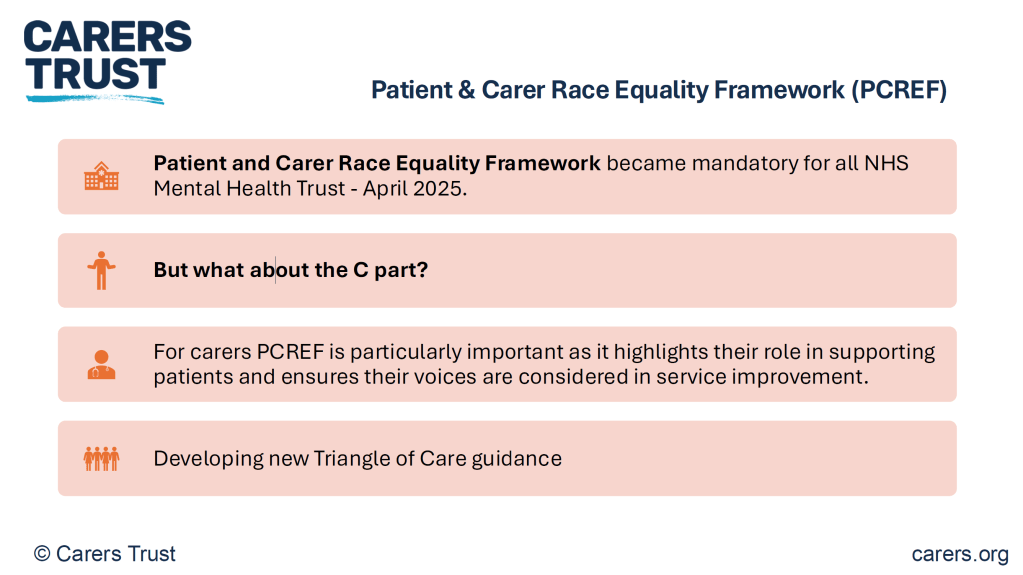
There was a particular focus on improving support for mental health carers in Lambeth. The Carers Hub Lambeth team continues to facilitate peer support groups and collaborates closely with the South London and Maudsley NHS Foundation Trust to ensure carers are recognised as partners in care planning. Initiatives like Triangle of Care are gaining momentum, emphasising better communication between professionals and families while creating pathways for carers to get involved in shaping local mental health services.
Carers Hub Lambeth also celebrated the growing range of community-based activities available for carers and families in Lambeth. Over the summer, there have been several events designed to support young carers, including trips, tours, and group workshops aimed at helping them connect with others and access emotional support. These initiatives are part of Lambeth’s broader goal to make sure younger carers, who are often overlooked, receive the help they need both at home and within education.
One of the key upcoming events for Lambeth carers is the Lambeth Carers Strategy Event taking place on 25th September 2025 at 336 Brixton Road. The session will bring together carers, professionals, and decision-makers to review plans, share ideas, and set priorities for the future. Carers are strongly encouraged to attend to ensure their voices are heard and to take part in shaping the borough’s action plans moving forward.
Southwark Council Carers Support and Strategy Group

Matthew fed back on how Southwark Council continues to strengthen its approach to supporting unpaid carers, with a growing emphasis on improving access to information, assessments, and respite services.
The Unpaid Carers Strategy Refresh is a project running from August 2025 to April 2026, led by Southwark Council in collaboration with Adult Social Care, the NHS, local voluntary groups, and unpaid carers themselves. The plan focuses on improving support for carers by updating evidence on local needs, strengthening engagement with seldom-heard groups, and mapping gaps in current services.
Key priorities include better access to respite care, enhanced referral pathways, stronger partnerships with health services, and improved inclusion of young carers, carers with disabilities, and LGBTQ+ carers. The initial phase, from August to October, involves reviewing existing strategies, mapping current services, gathering insights through focus groups and surveys, and benchmarking against national policies and neighbouring boroughs.
The forum highlighted the importance of co-production, ensuring that carers are actively involved in shaping local strategies and service priorities.
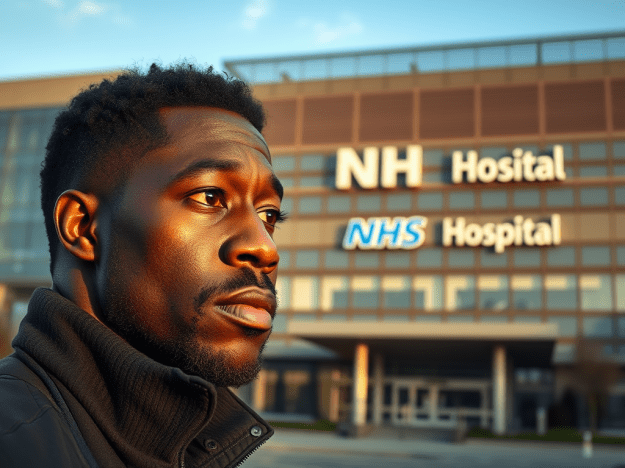
Update on Key Themes from the final NHS England Carers Conference

Matthew highlighted that the 2025 NHS England carers conference placed a strong emphasis on recognising unpaid carers as essential partners in delivering effective healthcare. The NHS stressed its commitment to involving carers in shaping services and policies, ensuring their voices are reflected at every stage of decision-making. There was a clear acknowledgement that without unpaid carers, many health and social care systems would face significant pressure.
You can watch the conference below.
A major focus was on the NHS’s shift towards neighbourhood-based care models designed to bring services closer to communities. Matthew explained that this change aims to improve coordination between GPs, hospitals, and mental health services, but he also highlighted concerns raised about fragmented communication and the risk of carers being left out of local planning. Carers at the conference called for better access to information and more joined-up pathways across boroughs.
The conference also featured interactive workshops and discussion groups focused on co-production, digital innovations, and addressing inequalities among carers. Specific sessions explored improving support for young carers, carers from minority backgrounds, and those supporting loved ones with mental health needs. The event closed with a call to action for stronger collaboration between carers, NHS teams, local authorities, and community organisations. Attendees were encouraged to get involved in upcoming forums and engagement opportunities to help shape future services and ensure carers’ voices are at the heart of decision-making.
Matthew shared updates on national policy developments discussed at the conference, including the Carers Leave Act and commitments to expanding access to respite, assessments, and flexible working rights. There was also a discussion about new digital tools and support platforms designed to make it easier for carers to connect with professionals and access resources. However, many attendees expressed concerns that these initiatives need proper funding and training to work effectively in practice.