By Matthew McKenzie, Co-Facilitator – SW London Carers Forum
About the South West London Carers Group
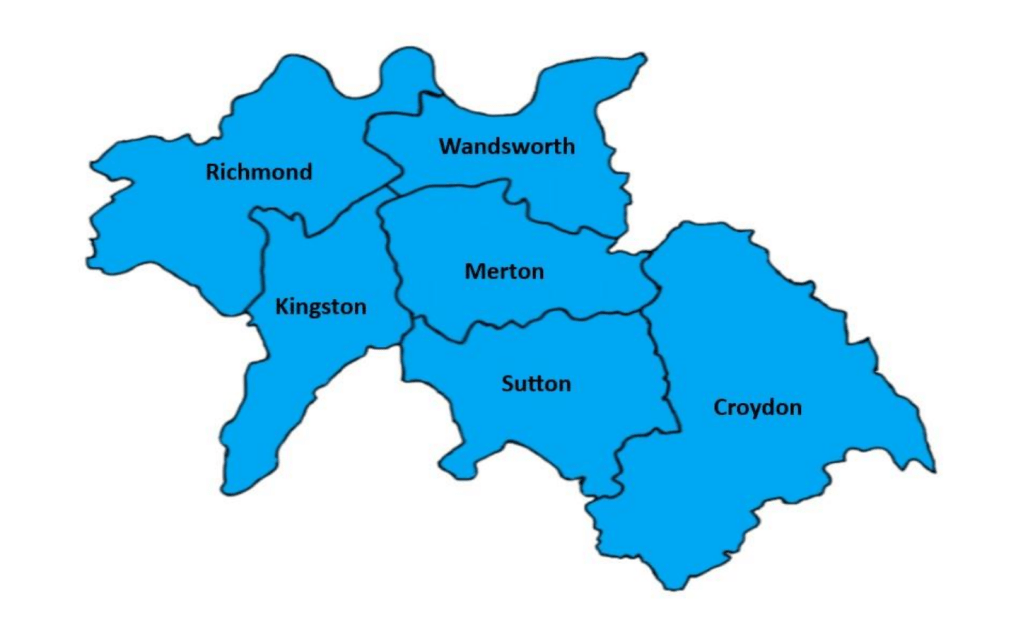
The South West London Carers Group brings together unpaid mental health carers from across the boroughs of Sutton, Merton, Wandsworth, Richmond and Kingston, to share experiences, gain peer support, and stay informed about local health and social care developments.
The group provides a safe and welcoming space where carers can discuss the challenges of supporting loved ones particularly those with long-term conditions or mental health needs while also learning from guest speakers, professionals, and each other. Co-facilitated by myself, the forum plays an important role in making carers’ voices heard and strengthening connections between carers and local NHS, mental health, and community services.
Our November South West London Carers Group meeting brought one of the most informative sessions we’ve had all year. We were joined by Dalvinder, the Patient Experience Lead for NHS 111, who provided a thorough and eye-opening look at how the 111 urgent care service really works, what carers can expect, and how the system is evolving.
Dal’s role involves reviewing patient feedback, monitoring the quality of calls, and ensuring that the service remains compassionate, safe, and responsive. He also regularly meets with community groups, like ours to raise awareness of what 111 can offer.
24/7 Telephone Assessments
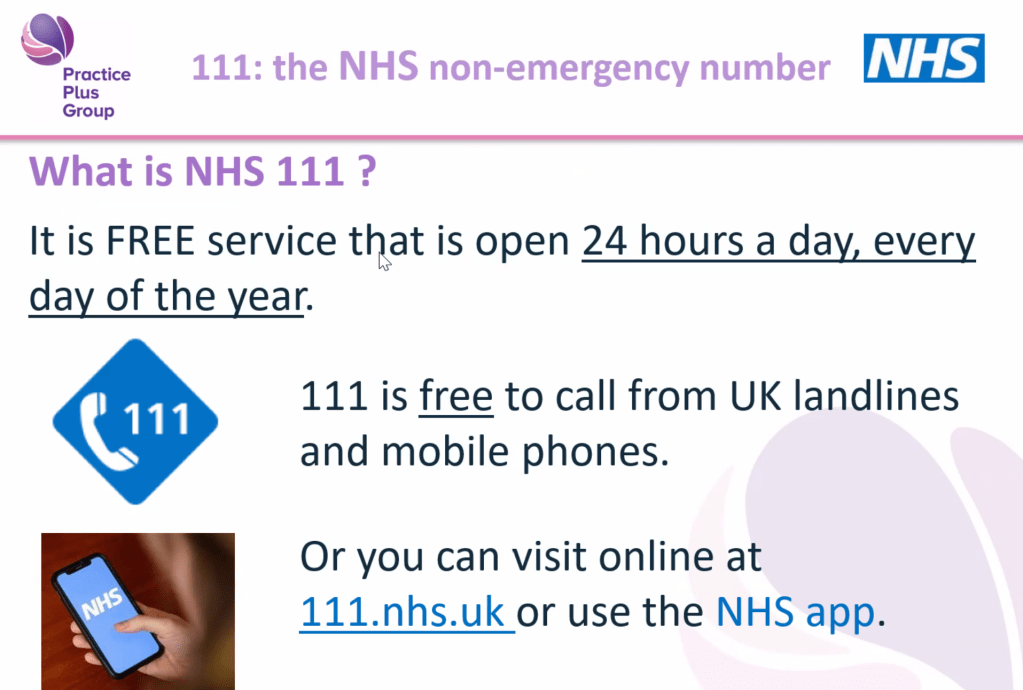
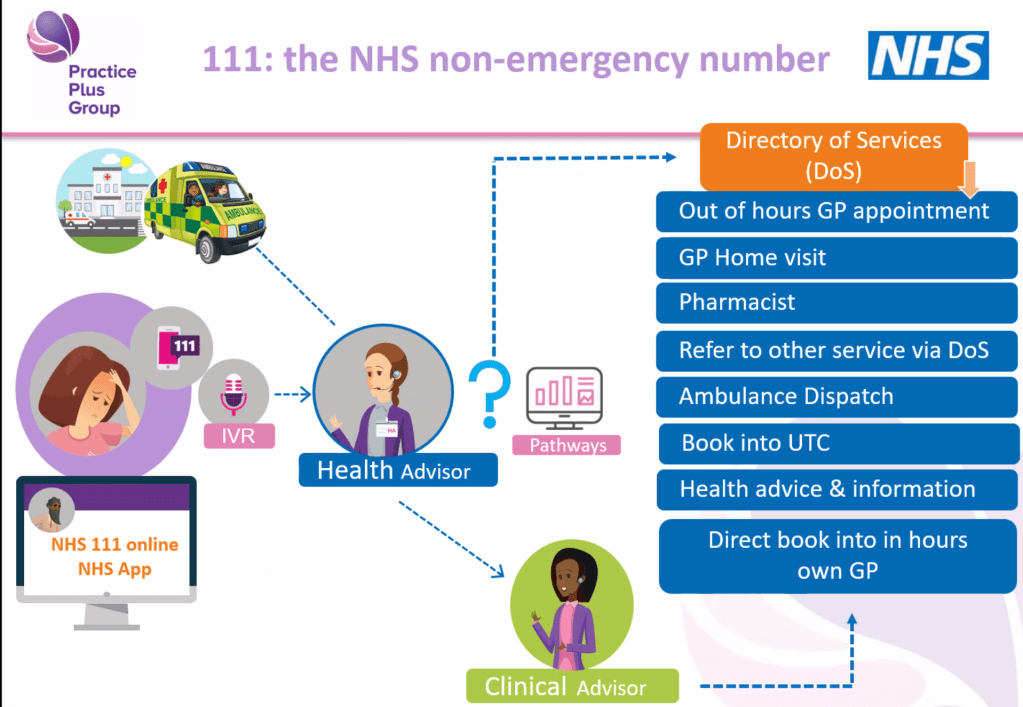
Dal opened by reminding us that NHS 111 operates 24 hours a day, 365 days a year, and never closes. The telephone assessment is often the first point of contact, and callers speak to a trained health advisor who uses the NHS Pathways system to ask structured questions. This ensures the call handler can rule out serious issues and direct the caller to the right service quickly. Dal emphasised that while questions can feel detailed or repetitive, each answer opens or closes clinical “pathways,” helping the system determine the safest next step.
GP Home Visiting (Evenings, Overnights, Weekends)
One of the biggest surprises for many carers was learning that NHS 111 has a GP home visiting service, specifically for times when GP surgeries are closed weekday evenings, overnight, weekends, and bank holidays. This service is intended for people who cannot safely travel, including those with mobility issues, caring responsibilities, or urgent health needs that don’t require hospital care. If a home visit is determined to be appropriate, a GP working for 111 can visit in a dedicated GP car and may provide medication on the spot or issue prescriptions if needed.
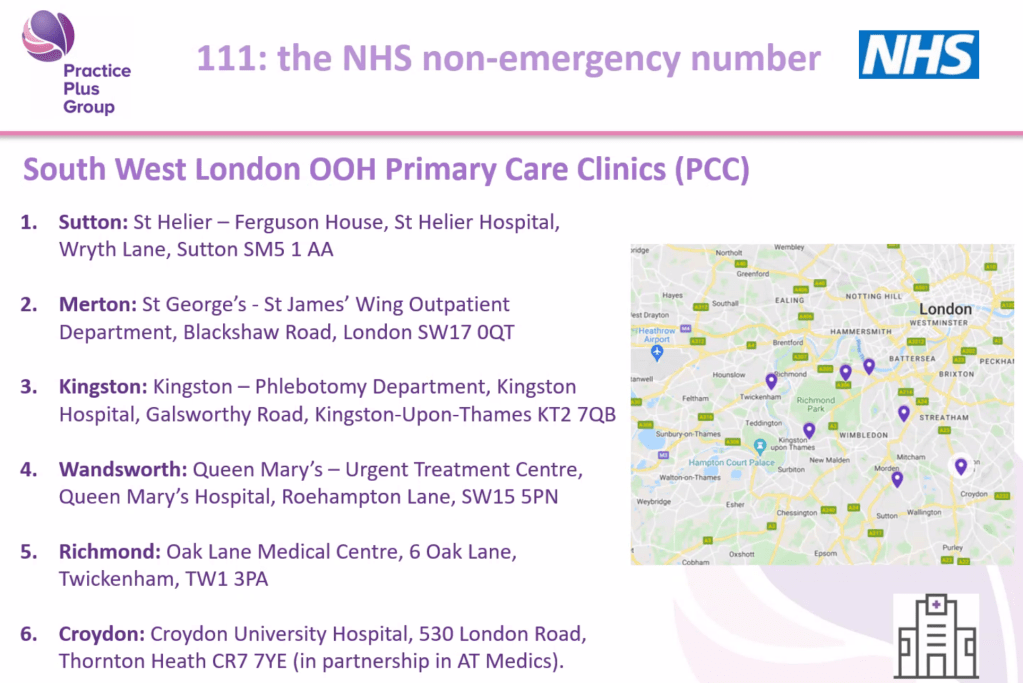
Primary Care Clinics (PCCs) – Same-Day Appointments via 111
Dal also explained the role of Primary Care Clinics (PCCs) located across South West London. These clinics operate outside normal GP hours and can see patients the same day—but crucially, access is by 111 referral only. If 111 decides that someone needs to see a GP face-to-face and can travel, they may be booked into a PCC appointment. Carers learned that you cannot walk into these clinics directly; 111 must assess the situation and confirm the appointment. This helps manage demand and ensures that appointments go to those who need them most urgently.
The Expanding Role of Pharmacies and “Pharmacy First”
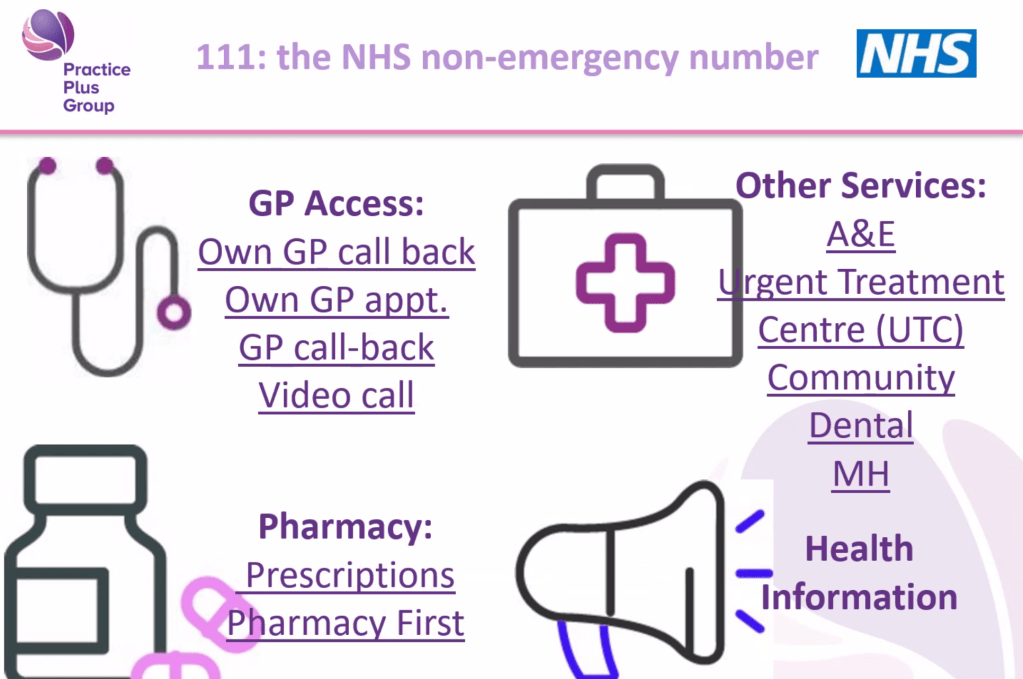
Another major theme was the evolving role of pharmacies in urgent care. Dal explained that pharmacists are highly trained professionals—more trained than many realise—and 111 can now direct callers to pharmacists for assessments, repeat prescriptions, and urgent medication needs. The Pharmacy First scheme allows some pharmacies to provide consultations and treatment in private rooms for a range of minor illnesses. 111 can also arrange emergency prescription access if someone runs out of routine medication while travelling, provided the medication is part of their regular treatment.
Arranging Call-Backs From Your Own GP
In certain situations, NHS 111 can request that your own GP practice contacts you, especially for non-face-to-face issues such as renewal of regular medication, questions about paperwork, or administrative needs. While GP appointment slots reserved for 111 are limited and fill quickly, the service can still send urgent notifications to GP surgeries when clinically necessary. Dal encouraged carers to mention when the need is time-sensitive so the system can prioritise appropriately.
Mental Health Support via 111 Option 2
One of the most important updates for mental health carers was the introduction of 111 Option 2, currently being trialled across London. When callers choose this option, the call is diverted away from standard 111 and straight to local specialist mental health teams, who can assess issues such as relapse, agitation, distress, changes in behaviour, or crises at home. Dal emphasised that while 111 is not a specialist mental health service, Option 2 ensures that people with mental health needs receive expert support. Data from the pilot is expected next year, and Dal offered to return to share the outcomes.
What We Learned About NHS 111
Many carers know the NHS 111 number exists, but few realise the range of services behind it. Dal explained that 111 is a free, 24/7 service (including weekends and holidays) designed for urgent health concerns that are not life-threatening.
Many carers commented that they had no idea 111 provided such a broad range of services.
Questions From Carers
Carers asked many thoughtful and practical questions during the session, including:
1. Mental Health Crises
A carer asked how 111 responds to mental health emergencies, particularly when someone becomes distressed, unwell, or difficult to support at home.
Dal explained that 111 itself is a generic urgent care service, but Option 2 sends callers straight to trained mental health professionals, who can triage cases such as relapse, agitation, or risk concerns in a more specialist way.
2. Access to Medical Records
A question was raised about whether 111’s clinicians can view a patient’s medical history.
Dal clarified that clinicians have access to the Summary Care Record, containing essential medical information, medications, conditions, and recent interactions—if the caller gives consent.
3. Home Visiting Times and Coverage
Carers asked about response times and geographical limits.
Dal explained that SW London is fully covered, though travel times vary depending on the area and how busy the service is. Home visiting is evenings, nights, and weekends only.
4. Staffing Levels and Training
One question focused on whether call handlers are medically trained.
Dal shared that 111 employs 180 health advisors in SW London—non-clinical staff who have completed an intensive six-week training program. They follow the NHS Pathways system and are supported by clinical advisors (GPs, nurses, paramedics) who can join or take over calls when needed.
5. Using 111 When Travelling
A carer asked about getting medication while away from home.
Dal explained that 111 can arrange for prescription collections at pharmacies in another part of England, which has helped many travellers who forget medication.
6. Hearing Impairment and Accessibility
There was interest in support for people who cannot make phone calls.
Dal confirmed services such as text relay, online 111, and the NHS App, all of which improve accessibility for carers and patients with additional needs.
Carer Reflections and Experiences
Several carers shared personal experiences both positive and challenging. One described how 111 triage was vital when they urgently needed treatment for a severe infection, while another discussed difficulties when GP surgeries didn’t always respond quickly to reports sent by 111.
These real stories helped emphasise how important it is for carers to know when and how to use the service, and how essential accurate information is during triage.
Key Tips Dal Shared for Carers
- Give as much information as possible, including social factors such as caring responsibilities, mobility challenges, or inability to travel.
- Stay with the person you’re calling about, as the call handler will ask you to check symptoms in real time.
- Tell 111 if symptoms change—this can alter the urgency and outcome.
- Always keep your phone nearby when waiting for a callback; 111 will try only three times.
- Don’t hesitate to call again if you’re unsure or worried.
Closing Thoughts
The session was incredibly well-received. Many carers said they learned things they never knew, even though they had used 111 before. Dal’s openness and honesty—both about what the service can do and what its limitations are—made his presentation especially valuable.
As co-facilitator, I (Matthew McKenzie) will continue to share information like this to help carers navigate local health services more confidently. We hope to invite Dal back once the evaluation of 111 Option 2 (mental health) is published, we also have a keen interest on what the ICB is doing especially regarding carer involvement.